Hello friends! Here are notes and detailed explanations for questions and answers to the NBME internal medicine Form 4 practice exam. Hope this helps and good luck! Check out the answers and explanations for NBME internal medicine Form 6 practice exam here.
An X-ray of the chest is a radiographic examination used to visualize the structures within the chest cavity, including the heart, lungs, and surrounding tissues. Clubbing of fingers and toes, a condition where the fingertips and toes appear enlarged and the nails curve around the fingertips, is a characteristic sign of hypertrophic osteoarthropathy. This condition is often associated with underlying pulmonary or cardiovascular diseases.
Hypercarbia refers to an excess of carbon dioxide (CO2) in the bloodstream, typically resulting from inadequate ventilation. Oxygen supplementation can sometimes lead to a decrease in respiratory drive, causing the retention of CO2 and exacerbating hypercarbia. This condition can be particularly concerning in patients with respiratory compromise, such as chronic obstructive pulmonary disease (COPD).
Mycoplasma pneumoniae is a type of atypical bacteria known to cause respiratory infections, particularly in young individuals. Symptoms typically include a non-productive cough, low-grade fever, and patchy or diffuse interstitial infiltrates on chest X-ray. Despite the severity of lung involvement seen on imaging, patients often report feeling less ill than expected, hence the adage that “the CXR looks worse than the patient feels.”
Legionella pneumophila is a bacterium responsible for causing Legionnaires’ disease, a severe form of pneumonia often accompanied by gastrointestinal symptoms such as diarrhea. One of the hallmark clinical features is pulse temperature dissociation, where patients exhibit fever disproportionate to their heart rate. Prompt recognition and treatment are crucial due to the potential for rapid clinical deterioration.
Renal artery stenosis (RAS) occurs when the arteries supplying the kidneys become narrowed, often due to atherosclerosis. The presence of a carotid bruit, an abnormal sound heard over the carotid artery indicative of turbulent blood flow, may suggest atherosclerosis elsewhere in the vascular system. In cases where atherosclerosis affects multiple vessels, it’s more likely to lead to RAS, highlighting the importance of considering systemic vascular disease in the diagnostic evaluation.
Erythropoietin is a hormone produced primarily by the kidneys and essential for red blood cell production. In conditions such as chronic kidney disease (CKD), where renal function is compromised, there is decreased production of erythropoietin, leading to anemia. A corrected reticulocyte count of approximately 1.2% suggests inadequate bone marrow stimulation, further corroborating the diagnosis of erythropoietin deficiency anemia in the setting of CKD.
Pamidronate is a bisphosphonate medication used in the long-term treatment of hypercalcemia, a condition characterized by elevated levels of calcium in the blood. Short-term management often involves intravenous fluids and calcitonin to promote calcium excretion. However, for sustained control of hypercalcemia, bisphosphonates like pamidronate are preferred due to their ability to inhibit bone resorption and reduce calcium levels over time.
Drug-induced neutropenia can occur as a side effect of certain medications, such as propylthiouracil (PTU) and methimazole, which are used in the treatment of hyperthyroidism. Neutropenia is characterized by a decreased number of neutrophils in the blood, predisposing individuals to infections. Monitoring blood counts regularly is essential when using these medications to promptly identify and manage neutropenia if it occurs.
Villous atrophy in the small bowel refers to the flattening of the tiny hair-like projections called villi that line the intestinal wall. D-xylose absorption test, which evaluates the absorption of a simple sugar in the proximal small bowel, depends solely on the presence of intact mucosa rather than enzymatic breakdown. In conditions like celiac disease, where there is villous blunting due to autoimmune-mediated damage, D-xylose absorption is impaired, contributing to malabsorption and gastrointestinal symptoms.
The initiation of three-drug antiretroviral therapy (ART) is recommended for individuals diagnosed with HIV regardless of their CD4 count. Using a combination of at least three antiretroviral drugs is essential to suppress viral replication effectively and prevent the emergence of drug-resistant strains. With the advent of highly active antiretroviral therapy (HAART), the need for prophylaxis against opportunistic infections like Pneumocystis jiroveci pneumonia is diminished in patients with CD4 counts above 200 cells/mm³, as immune function improves with viral suppression.
Direct current countershock, also known as DC cardioversion, is a medical procedure used to convert certain abnormal heart rhythms back to normal sinus rhythm. In the context of a wide QRS complex, it is indicative of ventricular tachycardia, a potentially life-threatening arrhythmia. Administering a shock is often necessary to restore the heart’s rhythm to a stable state. This intervention requires careful monitoring and coordination to deliver the appropriate energy level and timing for effective cardioversion without causing harm to the patient’s cardiac function.
Choledocholithiasis refers to the presence of gallstones in the common bile duct, obstructing the flow of bile from the liver to the intestines. Elevated levels of amylase suggest pancreatic involvement, indicating a possible blockage at the pancreatic duct due to reflux of bile into the pancreatic duct. Similarly, increased direct bilirubin levels suggest obstruction of the common bile duct, causing impaired bile excretion. These findings collectively point towards choledocholithiasis as the underlying pathology, necessitating further diagnostic evaluation and potentially therapeutic interventions such as endoscopic retrograde cholangiopancreatography (ERCP) for stone removal.
The left medial longitudinal fasciculus (MLF) is a pathway within the brainstem responsible for coordinating eye movements, particularly in conjugate gaze. Dysfunction of the left MLF can lead to a characteristic clinical finding known as internuclear ophthalmoplegia (INO), where there is weakness of adduction in the eye on the affected side during lateral gaze. This occurs because the MLF connects the ipsilateral paramedian pontine reticular formation (PPRF) with the contralateral oculomotor nucleus, facilitating coordinated eye movements. Identifying this deficit clinically helps localize lesions within the brainstem and aids in diagnosing conditions such as multiple sclerosis.
Calcification of a bicuspid aortic valve is a congenital anomaly that predisposes individuals to aortic stenosis, a condition characterized by narrowing of the aortic valve opening. In younger patients, the presence of a systolic ejection murmur suggests a congenital cause, as acquired valvular diseases typically manifest later in life. The increased resistance to blood flow across the stenotic valve leads to left ventricular hypertrophy and stiffening, contributing to the development of an S4 heart sound. These findings highlight the importance of recognizing valvular abnormalities early in life and monitoring for complications such as aortic stenosis progression.
The supraspinatus tendon is one of the four tendons comprising the rotator cuff in the shoulder. Pathology involving the supraspinatus tendon often presents with characteristic symptoms such as pain over the lateral deltoid region, particularly exacerbated at night when lying on the affected shoulder. Additionally, pain elicited during abduction against resistance is a common clinical finding in rotator cuff pathology. These clinical features help differentiate rotator cuff disorders from other shoulder pathologies and guide further diagnostic evaluation and management strategies, including physical therapy, corticosteroid injections, or surgical intervention when indicated.
Acute tubular necrosis (ATN) is a type of kidney injury characterized by damage to the renal tubules, leading to impaired kidney function. It often manifests as a result of ischemic or nephrotoxic insults, such as severe hypotension or exposure to certain medications or toxins. The presence of significant blood in the urine (hematuria) without the presence of red blood cells (RBCs) on microscopic examination can indicate underlying rhabdomyolysis, a condition characterized by muscle breakdown. Myoglobin released from damaged muscle cells can cause myoglobinuria, leading to ATN as it obstructs renal tubules and impairs kidney function. Prompt recognition and management of the underlying cause are essential to prevent further kidney damage and facilitate renal recovery.
Seborrheic dermatitis is a common inflammatory skin condition characterized by red, greasy, and scaly patches, typically occurring on areas rich in sebaceous glands, such as the scalp, face (particularly around the eyebrows, nose, and ears), and upper chest. The rash often appears yellowish and may be associated with itching and discomfort. Seborrheic dermatitis has been linked to various factors, including HIV infection and Parkinson’s disease, although the exact mechanisms are not fully understood. Treatment typically involves topical antifungal or anti-inflammatory agents to alleviate symptoms and reduce inflammation.
The switch from heparin to direct thrombin inhibitor therapy may be necessitated by heparin-induced thrombocytopenia (HIT), a potentially serious immune-mediated complication of heparin therapy. HIT is characterized by a significant drop in platelet count and an increased risk of thrombosis. Management involves discontinuing all heparin products and initiating alternative anticoagulation therapy, such as a direct thrombin inhibitor (e.g., argatroban, bivalirudin) or fondaparinux. These agents directly inhibit thrombin without requiring antithrombin III and are not associated with cross-reactivity or platelet activation in HIT, making them suitable alternatives for anticoagulation in affected patients.
Gout is a form of inflammatory arthritis caused by the deposition of uric acid crystals in joints, leading to episodes of acute pain, swelling, and inflammation. Chronic alcohol use is a well-established risk factor for the development of gout, as alcohol consumption can lead to elevated uric acid levels by interfering with its metabolism and excretion. The characteristic presentation of gout often involves sudden onset of severe joint pain, commonly affecting the big toe (podagra), although it can involve other joints as well. Management typically includes lifestyle modifications, such as dietary changes and reducing alcohol intake, along with pharmacological interventions to alleviate pain and lower uric acid levels.
Magnetic resonance imaging (MRI) of the lumbosacral spine is a non-invasive imaging modality used to evaluate various conditions affecting the lower back and spinal cord, including nerve root compression. Compression of the sacral nerves by a tumor or other structural abnormalities can result in a clinical syndrome known as cauda equina syndrome (CES). CES is characterized by bilateral paralysis and numbness of the lower extremities, urinary incontinence (typically overflow incontinence), saddle anesthesia (loss of sensation in the perineal area), and absent deep tendon reflexes (DTRs) below the knee. MRI is considered the imaging modality of choice for diagnosing nerve root compression and identifying the underlying cause, guiding appropriate management strategies such as surgical intervention or medical therapy.
α1-antitrypsin deficiency is a genetic condition characterized by a deficiency of the α1-antitrypsin protein, which plays a crucial role in protecting the lungs from damage caused by enzymes released by inflammatory cells. In affected individuals, the lack of this protein predisposes them to develop panacinar emphysema, a type of emphysema that involves the destruction of the alveoli throughout the entire lung, resulting in increased lung lucency particularly prominent at the lung bases on imaging studies such as chest X-rays or CT scans. This emphysematous change is often seen in younger patients and can lead to symptoms such as shortness of breath, coughing, and wheezing. Early detection and management, including smoking cessation and, in some cases, augmentation therapy with α1-antitrypsin, are crucial in slowing the progression of lung damage in individuals with this deficiency.
Hodgkin’s disease is a type of lymphoma characterized by the presence of Reed-Sternberg cells within the lymph nodes. Clinical features such as a single enlarged lymph node, pruritus (itching), and the absence of pharyngeal erythema make Hodgkin’s disease more likely than infectious mononucleosis. Unlike many other lymphomas, Hodgkin’s disease tends to involve a single lymph node or a localized group of lymph nodes initially. Furthermore, the leukocyte count is typically not elevated in Hodgkin’s disease as the pathological lymphocytes are confined to the affected nodes, unless there is a leukemic transformation. Diagnosis involves lymph node biopsy and staging workup, followed by appropriate treatment modalities such as chemotherapy and radiation therapy.
The addition of lisinopril to the medication regimen is indicated in certain clinical scenarios, particularly in patients with diabetes mellitus (DM) and associated nephropathy. Lisinopril, an angiotensin-converting enzyme inhibitor (ACEi), helps to reduce glomerular hyperfiltration and proteinuria associated with diabetic nephropathy, thereby slowing the progression of renal disease. By inhibiting the conversion of angiotensin I to angiotensin II, lisinopril helps to dilate blood vessels and decrease blood pressure, thus protecting the kidneys from further damage. Close monitoring of renal function and electrolytes is essential when initiating lisinopril therapy, particularly in patients with pre-existing renal impairment or on concurrent medications that affect renal function.
Lisinopril therapy is often initiated in patients with hypertension (HTN) to reduce the risk of cardiovascular events such as stroke and heart attack. Hypertensive hemorrhagic strokes are common complications of uncontrolled HTN, emphasizing the importance of aggressive blood pressure control. Lifestyle modifications, including weight reduction, are recommended as adjuncts to pharmacotherapy; however, in patients with a history of complications from HTN, such as stroke, prompt initiation of antihypertensive medication like lisinopril is essential. While weight reduction can lead to significant reductions in blood pressure, it may not be sufficient on its own in patients with established vascular complications, necessitating pharmacological intervention to achieve target blood pressure goals and mitigate further risks.
Nonketotic hyperosmolar state (HHS) is a serious and life-threatening complication of diabetes mellitus characterized by profound hyperglycemia (>600 mg/dL), marked dehydration, and hyperosmolality without significant ketoacidosis. Unlike diabetic ketoacidosis (DKA), which is more commonly associated with type 1 diabetes, HHS typically occurs in patients with type 2 diabetes, often in the setting of concurrent illness or infection. The absence of significant ketosis in HHS is attributed to sufficient insulin levels to inhibit lipolysis and ketogenesis but insufficient to facilitate glucose utilization, leading to severe hyperglycemia and osmotic diuresis. Prompt recognition and aggressive fluid and electrolyte replacement are crucial in the management of HHS to prevent complications such as cardiovascular collapse, renal failure, and central nervous system dysfunction.
Autoinfection refers to the process by which an individual becomes reinfected with the same pathogen, typically due to poor hygiene practices or failure to eliminate the source of infection. For instance, in the case of a fungal infection such as athlete’s foot, scratching the affected area and then inadvertently touching the groin area can transfer fungal spores, leading to reinfection in a new location. In this scenario, the individual essentially serves as their own source of infection. It’s important to note that resistance to treatment is unlikely if the rash resolved with initial therapy, suggesting that the same treatment approach may be effective in managing the reinfection. However, preventive measures such as proper hygiene and avoidance of scratching can help minimize the risk of autoinfection and recurrence of the condition.
Autonomous T4 production typically occurs in the context of a thyroid nodule, specifically a toxic adenoma. In this condition, the thyroid nodule becomes independent of the normal regulatory mechanisms that govern thyroid hormone production and secretion. As a result, the adenoma autonomously produces and releases excessive amounts of thyroxine (T4), leading to hyperthyroidism. Toxic adenomas can present with symptoms such as palpitations, heat intolerance, weight loss, and tremors. Diagnosis is often confirmed through thyroid function tests and imaging studies, with treatment options including antithyroid medications, radioactive iodine therapy, or surgical resection depending on the individual’s clinical presentation and preferences.
Discharging a patient home with home hospice care is a compassionate approach often taken in end-of-life situations, particularly for individuals with advanced stage IV non-small cell lung carcinoma (NSCLC). Stage IV NSCLC typically indicates metastatic disease with a poor prognosis, and without active treatment, the median life expectancy is often less than six months. Hospice care focuses on providing comfort and supportive care to patients and their families, managing symptoms, and improving quality of life during the end-of-life phase. This decision involves discussions between healthcare providers, patients, and their families to ensure alignment with the patient’s goals of care and preferences.
Upper endoscopy, also known as esophagogastroduodenoscopy (EGD), is a diagnostic procedure used to visualize the upper gastrointestinal tract, including the esophagus, stomach, and duodenum. It is indicated in patients with alarm symptoms such as dysphagia (difficulty swallowing), unexplained weight loss, or anemia, which may suggest underlying gastrointestinal pathology such as esophageal strictures, tumors, peptic ulcers, or gastrointestinal bleeding. During the procedure, a flexible endoscope is passed through the mouth and advanced into the upper digestive tract, allowing for direct visualization of the mucosal lining and biopsy of suspicious lesions if necessary. Upper endoscopy plays a crucial role in the evaluation of various upper gastrointestinal disorders and guiding appropriate management strategies.
Rhabdomyolysis is a serious medical condition characterized by the breakdown of skeletal muscle tissue, leading to the release of myoglobin into the bloodstream and subsequent myoglobinuria. The presence of 2+ blood on urine dipstick without red blood cells (RBCs) is indicative of myoglobinuria, a hallmark feature of rhabdomyolysis. This condition can be triggered by various factors such as trauma, prolonged immobilization, muscle ischemia, exertion, or certain medications and toxins. Rhabdomyolysis can result in electrolyte imbalances, acute kidney injury, and even life-threatening complications such as compartment syndrome or disseminated intravascular coagulation (DIC). Prompt recognition and management, including aggressive fluid resuscitation and treatment of underlying causes, are essential in preventing complications and promoting recovery.
Managing anticoagulation in patients with a prosthetic aortic valve poses unique challenges due to the increased risk of thromboembolic events associated with mechanical valves. Compared to adenocarcinoma or other hypercoagulable states, prosthetic valves require higher international normalized ratio (INR) targets to reduce the risk of valve thrombosis and embolism. This higher INR target aims to prevent clot formation on the valve surfaces, minimizing the risk of systemic embolization, stroke, or valve dysfunction. The mechanical nature of prosthetic valves creates an environment prone to thrombus formation, underscoring the importance of vigilant anticoagulation therapy and regular monitoring to maintain therapeutic levels and reduce the risk of complications.
Fine-needle aspiration (FNA) of a lesion is a minimally invasive diagnostic procedure commonly used to obtain tissue samples for cytological analysis, particularly in cases suspicious for malignancy. Risk factors for cancer, such as a history of smoking, family history of cancer, or concerning imaging findings, warrant further investigation through FNA to establish a definitive diagnosis. Additionally, thyroid nodules associated with normal or elevated thyroid-stimulating hormone (TSH) levels may harbor malignant potential and necessitate cytological evaluation via FNA. However, in cases of low TSH levels, further imaging studies such as iodine 123 scintigraphy may be indicated to differentiate between benign and malignant thyroid nodules and guide subsequent management strategies.
Weight loss can have a beneficial effect on joint health by reducing pressure on weight-bearing joints, thus lowering the risk of developing osteoarthritis (OA) or alleviating symptoms in individuals with pre-existing OA. Excess body weight places increased mechanical stress on joints, accelerating cartilage degeneration and contributing to the progression of OA. Therefore, weight loss interventions aimed at reducing body mass index (BMI) can help alleviate symptoms and improve functional outcomes in individuals with OA. Implementing lifestyle modifications such as dietary changes and regular physical activity can aid in achieving sustainable weight loss and optimizing joint health in both preventive and therapeutic contexts.
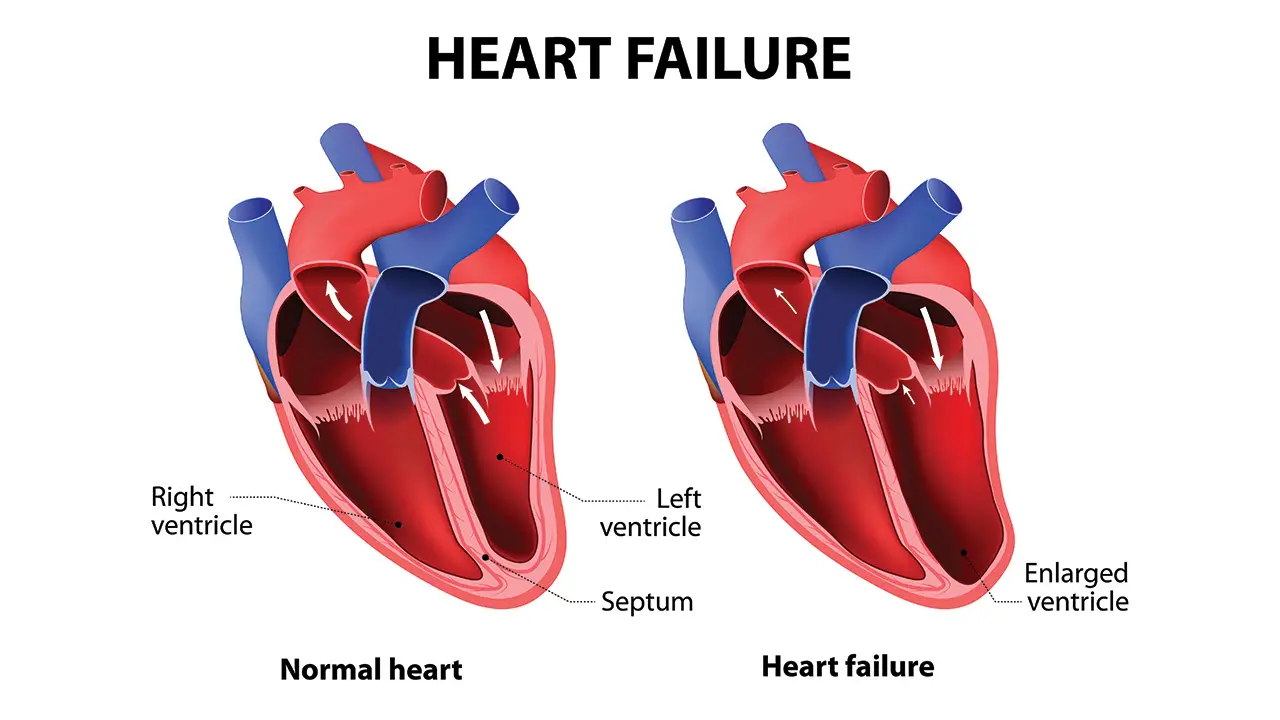
Prerenal azotemia is a form of acute kidney injury characterized by reduced renal perfusion leading to impaired glomerular filtration and subsequent elevation of blood urea nitrogen (BUN) and serum creatinine (Cr) levels. Diagnostic criteria for prerenal azotemia typically include a urine sodium (Na) concentration of less than 10 mEq/L, fractional excretion of sodium (FENa) of less than 1%, and a BUN/Cr ratio greater than 20. These laboratory findings indicate decreased renal blood flow and effective volume depletion, commonly seen in conditions such as hypovolemia, dehydration, or heart failure. Prompt identification and management of the underlying cause of prerenal azotemia are crucial to prevent further renal injury and restore renal function.
Obstruction of the small bowel can present with varying degrees of bowel movement alterations, with increased bowel movements often indicative of small bowel obstruction (SBO) and decreased or absent bowel movements suggestive of ileus. Patients with a history of multiple bowel procedures, such as abdominal surgeries or inflammatory bowel disease, are at increased risk of developing adhesive SBO, which occurs due to the formation of scar tissue and adhesions that can obstruct the bowel lumen. Adhesions are recognized as the leading cause of SBO, highlighting the importance of considering prior surgical history in the evaluation of bowel obstruction and guiding appropriate management strategies, which may include conservative measures or surgical intervention depending on the severity and underlying etiology.
Paroxysmal ventricular tachycardia (PVT) is a type of abnormal heart rhythm originating from the ventricles, typically characterized by rapid, regular heartbeats arising suddenly and intermittently. In patients with a history of heart disease, such as previous myocardial infarction (MI), the presence of abnormal ECG findings, including Q waves indicative of prior myocardial injury, raises suspicion for a cardiac etiology of PVT. This underscores the importance of comprehensive cardiac evaluation, including echocardiography and coronary angiography, to assess for structural heart abnormalities and ischemic changes that may predispose to arrhythmias. Prompt recognition and management of PVT are essential to prevent hemodynamic compromise and potential complications such as syncope, heart failure, or even sudden cardiac death.
Influenza virus vaccination is recommended annually, especially for individuals at higher risk of severe influenza-related complications, such as the elderly, young children, pregnant women, and individuals with underlying medical conditions. Annual vaccination helps ensure ongoing protection against influenza strains that may vary from year to year and helps to reduce the spread of the virus within the community. By stimulating the immune system to produce antibodies against specific influenza strains, vaccination can significantly reduce the risk of influenza infection, lessen the severity of illness if infection occurs, and prevent influenza-related hospitalizations and deaths. Routine influenza vaccination is a key component of public health efforts to control seasonal influenza outbreaks and protect vulnerable populations.
Increasing the dose of lisinopril, an angiotensin-converting enzyme (ACE) inhibitor, may be warranted in patients with persistent hypertension despite initial therapy. Lisinopril not only helps lower blood pressure but also exerts kidney-protective effects, particularly in patients with chronic kidney disease or diabetic nephropathy. In individuals whose blood pressure remains above the target range (e.g., <140/90 mmHg), despite initial lisinopril therapy, dose escalation or combination therapy with other antihypertensive agents may be necessary to achieve optimal blood pressure control and reduce the risk of cardiovascular events and progressive kidney damage. Close monitoring of renal function, electrolytes, and blood pressure is essential when titrating lisinopril dosage to minimize the risk of adverse effects while maximizing therapeutic benefit.
Atrial septal defect (ASD) is a congenital heart defect characterized by an abnormal opening in the atrial septum that allows shunting of blood between the atria. The presence of a fixed split second heart sound (S2) on auscultation is a classic physical finding in patients with ASD. This fixed split S2 results from delayed closure of the pulmonic valve due to increased blood flow to the right heart chambers during both inspiration and expiration. Diagnosis of ASD typically involves echocardiography to visualize the defect and assess its size and hemodynamic significance. While small ASDs may be asymptomatic and require no intervention, larger defects may necessitate surgical or transcatheter closure to prevent complications such as pulmonary hypertension, right-sided heart failure, and paradoxical embolism.
Decreased vascular compliance refers to the reduced ability of blood vessels to expand and contract in response to changes in blood volume or pressure. With increasing age, there is a natural stiffening of the arterial walls due to changes in the composition and structure of vascular tissues, including collagen deposition and elastin degradation. This age-related decrease in vascular compliance contributes to elevated systolic blood pressure, widened pulse pressure, and increased cardiovascular risk. Impaired vascular compliance can also impair tissue perfusion, increase cardiac workload, and predispose to target organ damage, including stroke, myocardial infarction, and renal dysfunction. Lifestyle modifications, such as regular exercise, smoking cessation, and dietary changes, along with pharmacological interventions targeting blood pressure and vascular health, can help mitigate the adverse effects of decreased vascular compliance and reduce cardiovascular risk in older adults.
Debridement of an ulcer is a crucial aspect of wound care management, particularly in cases where necrotic tissue, known as eschar, has formed over the wound bed. Removal of eschar through debridement facilitates wound healing by eliminating a barrier to tissue repair, reducing the risk of infection, and promoting granulation tissue formation. Debridement can be achieved through various methods, including surgical, mechanical, enzymatic, or autolytic, depending on the nature and extent of the wound. By clearing away necrotic tissue, debridement creates a clean wound bed conducive to cellular proliferation and re-epithelialization. Additionally, debridement allows for better visualization and assessment of the wound, guiding subsequent treatment strategies to optimize wound healing outcomes.
Chlamydia trachomatis is a sexually transmitted bacterium responsible for a range of infections, including genital, ocular, and respiratory tract infections. Unlike many bacteria, chlamydia cannot be visualized using Gram staining techniques due to its unique cell wall composition. Instead, the diagnosis of chlamydial infections typically relies on specialized staining methods such as Giemsa stain or immunofluorescence microscopy to visualize intracellular chlamydial inclusions within host cells. Differential diagnosis between chlamydial and other sexually transmitted infections, such as Neisseria gonorrhoeae, can be made based on the absence of intracellular organisms on microscopic examination. Timely and accurate diagnosis of chlamydial infections is essential for prompt initiation of appropriate antibiotic therapy and prevention of complications such as pelvic inflammatory disease and infertility.
Oral contraceptive therapy (OCPs) plays a pivotal role in the management of polycystic ovary syndrome (PCOS), a common endocrine disorder characterized by hormonal imbalances and ovarian dysfunction. OCPs containing both estrogen and progestin components help regulate menstrual cycles and reduce the risk of endometrial hyperplasia and carcinoma associated with unopposed estrogen exposure in women with PCOS. Additionally, OCPs can alleviate symptoms such as hirsutism, acne, and menstrual irregularities commonly seen in PCOS. For women with PCOS seeking fertility, alternative ovulation induction agents such as clomiphene citrate or metformin may be considered to induce ovulation and improve reproductive outcomes. Individualized treatment plans tailored to the patient’s reproductive goals and metabolic profile are essential in managing PCOS effectively.
Group B at year 3-4 refers to a specific cohort or subgroup within a longitudinal study, typically used in survival analysis to assess disease progression or treatment outcomes over time. In survival curves, the steepest negative slope indicates the greatest decline in survival rate within a given time period. Therefore, Group B at years 3-4 exhibits the most pronounced decrease in survival compared to other groups, indicating poorer survival rates or outcomes during this period. Understanding survival curves and interpreting slopes are critical in longitudinal studies to evaluate the effectiveness of interventions, prognosticate disease trajectories, and inform clinical decision-making.
Labetalol is a non-selective beta-blocker with alpha-blocking activity commonly used in the management of hypertension and hypertensive emergencies. By antagonizing beta-adrenergic receptors, labetalol reduces heart rate, cardiac output, and peripheral vascular resistance, leading to decreased blood pressure. Additionally, labetalol’s alpha-blocking properties contribute to vasodilation and further lower blood pressure by reducing aortic wall stress. In contrast, vasodilators such as nitroglycerin or hydralazine primarily lower blood pressure by directly dilating blood vessels, which can exacerbate aortic wall stress and potentially worsen conditions such as aortic dissection. Labetalol’s dual mechanism of action makes it a valuable option for managing hypertension in patients with concomitant cardiovascular conditions or aortic pathologies.
Laryngoscopy and endotracheal intubation are critical procedures used in emergency medicine, particularly in cases of upper airway obstruction such as epiglottitis, where the airway must be secured promptly to prevent respiratory compromise. Epiglottitis, often caused by bacterial infection, can lead to rapid onset of airway swelling and obstruction, posing a life-threatening situation. Laryngoscopy allows visualization of the larynx and epiglottis to confirm the diagnosis and assess the degree of airway compromise. Endotracheal intubation involves the insertion of a tube into the trachea to establish a patent airway and ensure adequate oxygenation and ventilation. These interventions should be performed with caution and under appropriate sedation to minimize the risk of further airway obstruction or complications, highlighting the importance of skilled airway management in emergent situations.
Quantitative immunoglobulin assay plays a crucial role in the evaluation of patients with chronic lymphocytic leukemia (CLL), a hematologic malignancy characterized by the proliferation of mature B lymphocytes. CLL is associated with immune dysregulation and hypogammaglobulinemia, which predisposes patients to recurrent infections and impaired humoral immunity. Quantitative measurement of immunoglobulin levels, including IgG, IgA, and IgM, helps assess the extent of hypogammaglobulinemia and guides therapeutic interventions such as immunoglobulin replacement therapy to reduce the risk of infections and improve clinical outcomes. Routine monitoring of immunoglobulin levels is essential in CLL management to detect and address immune deficiencies promptly, thereby optimizing patient care and reducing the morbidity associated with infectious complications.
Chest X-ray imaging is a valuable diagnostic tool in the evaluation of pulmonary barotrauma, a potential complication of diving-related activities such as scuba diving. Pulmonary barotrauma occurs when the diver fails to adequately exhale air during ascent, leading to overexpansion of gas within the lungs and subsequent alveolar rupture. This can result in the development of pneumothorax, pneumomediastinum, or subcutaneous emphysema, which can be detected on chest X-ray. Prompt recognition of pulmonary barotrauma on imaging allows for timely intervention and management, including decompression and supportive care to prevent further complications such as tension pneumothorax or respiratory distress. Chest X-ray findings play a crucial role in guiding treatment decisions and optimizing outcomes in individuals with diving-related injuries.
Endoscopic retrograde cholangiopancreatography (ERCP) is a therapeutic endoscopic procedure commonly used in the management of symptomatic pancreatic pseudocysts, a complication of acute or chronic pancreatitis. ERCP allows for direct visualization of the biliary and pancreatic ducts and enables therapeutic interventions such as drainage and stent placement to alleviate obstructive symptoms and prevent complications such as infection or rupture. Symptomatic pseudocysts, characterized by abdominal pain, jaundice, or evidence of ductal obstruction, are typically managed with ERCP-guided drainage procedures, which can be performed using various techniques such as cystgastrostomy or cystoduodenostomy. ERCP plays a pivotal role in the multidisciplinary approach to managing pancreatic pseudocysts, offering minimally invasive solutions and improving patient outcomes.
Diverticulitis is a common inflammatory condition of the colon, typically presenting with symptoms such as chronic constipation, left lower quadrant (LLQ) abdominal pain, tenderness, and potentially bloody stools or fever. The formation of diverticula, small pouches in the colon wall, predisposes individuals to diverticulitis, which occurs when these pouches become inflamed or infected. Chronic constipation and increased intraluminal pressure are significant risk factors for diverticulitis development. LLQ abdominal pain and tenderness are hallmark clinical features, often accompanied by systemic signs of inflammation such as fever and leukocytosis. Diagnosis is typically confirmed through imaging studies such as abdominal CT scans, and management involves a combination of antibiotics, pain management, and dietary modifications to relieve symptoms and prevent complications such as perforation or abscess formation.
Check out the answers and explanations for NBME internal medicine Form 6 practice exam here.
NBME 4, NBME 5, NBME 6 Internal Medicine Forms Answers and Explanations
Check out these popular articles
Circulatory System: Blood Flow Pathway Through the Heart
Ectoderm vs Endoderm vs Mesoderm
Circulatory System: Heart Structures and Functions
Ductus Arteriosus Vs Ductus Venosus Vs Foramen Ovale: Fetal Heart Circulation
Autocrine vs Paracrine vs Endocrine: What are the Differences?
Upper Vs Lower Respiratory System: Upper vs Lower Respiratory Tract Infections
Seven General Functions of the Respiratory System
Kidney Embryology & Development: Easy Lesson
Psychology 101: Crowd Psychology and The Theory of Gustave Le Bon
Cell Membrane Dynamics: Flippase Vs Floppase Vs Scramblase
Shoulder Abduction Muscles: Medical Anatomy and USMLE
Top Websites Like Sparknotes: 15 Free Sites and Resources Similar to Sparknotes
Cell Membrane Fluidity: Factors That Influence and Increase the Cell Membrane Fluidity
Copyright © 2024 Moosmosis Organization: All Rights Reserved
All rights reserved. This essay first published on moosmosis.org or any portion thereof may not be reproduced or used in any manner whatsoever
without the express written permission of the publisher at moosmosis.org.
Please Like and Subscribe for free to our Email List at moosmosis.org to support our open-access youth education initiatives!
Hello friends! Here are notes and detailed explanations for questions and answers to the NBME internal medicine Form 4 practice exam. Hope this helps and good luck! Check out the answers and explanations for NBME internal medicine Form 6 practice exam here. anatomy, Biology, cell biology, education, health, medicine, stem, technology, anemia, autonomic nervous system, bleeding, brain, brain bleed, brain stem, brain surgery, cardiologist, cardiology, central nervous system, cerebellum, cerebrum, college, ct head, ECG, epidural hematoma, gray matter, heart attack, heart failure, hemorrhage, hemorrhagic stroke, internal medicine, interventional radiology, ischemic stroke, life, mcat, medical, medical student, MRI, MRI brain, NBME Form 4, NBME Form 6, nerves, neurology, neuron, neuroradiology, neuroscience, neurosurgery, NMBE medicine, parasympathetic, peripheral nervous system, physiology, pre-medical, radiology, reflex, resident, school, science, somatosensory, STEP exam, stretch reflex, stroke, student, subarachnoid hemorrhage, subcortical cerebrum, subdural hematoma, surgery, sympathetic, TIA, transient ischemic attack, university, upper motor neuron, white matter Moosmosis