Hello friends! Here are notes and detailed explanations for questions and answers to the NBME internal medicine Form 5 practice exam. Hope this helps and good luck! Check out the answers and explanations for NBME internal medicine Form 6 practice exam here and NBME internal medicine Form 4 here.
Valvular insufficiency of deep veins occurs when the valves within the veins fail to function properly, leading to blood flowing backward instead of toward the heart. This condition often manifests with mild edema due to the pooling of blood caused by incompetent valves. Additionally, varicose veins can develop as a result of increased pressure and reflux of blood, particularly in the saphenous veins. A common finding is an area of hyperpigmentation, known as stasis dermatitis, which often appears over the ankles due to chronic venous insufficiency.
Not eating mahimahi, a type of dark-meat fish, can be a precautionary measure to avoid histamine toxicity, also known as scombroid poisoning. Consuming mahimahi, especially if improperly stored or prepared, can lead to symptoms resembling anaphylaxis due to the high levels of histamine present in the fish. These symptoms typically include flushing, headache, and light-headedness, and may also include urticaria and itching. Onset of symptoms usually occurs within 10 minutes of consuming the fish.
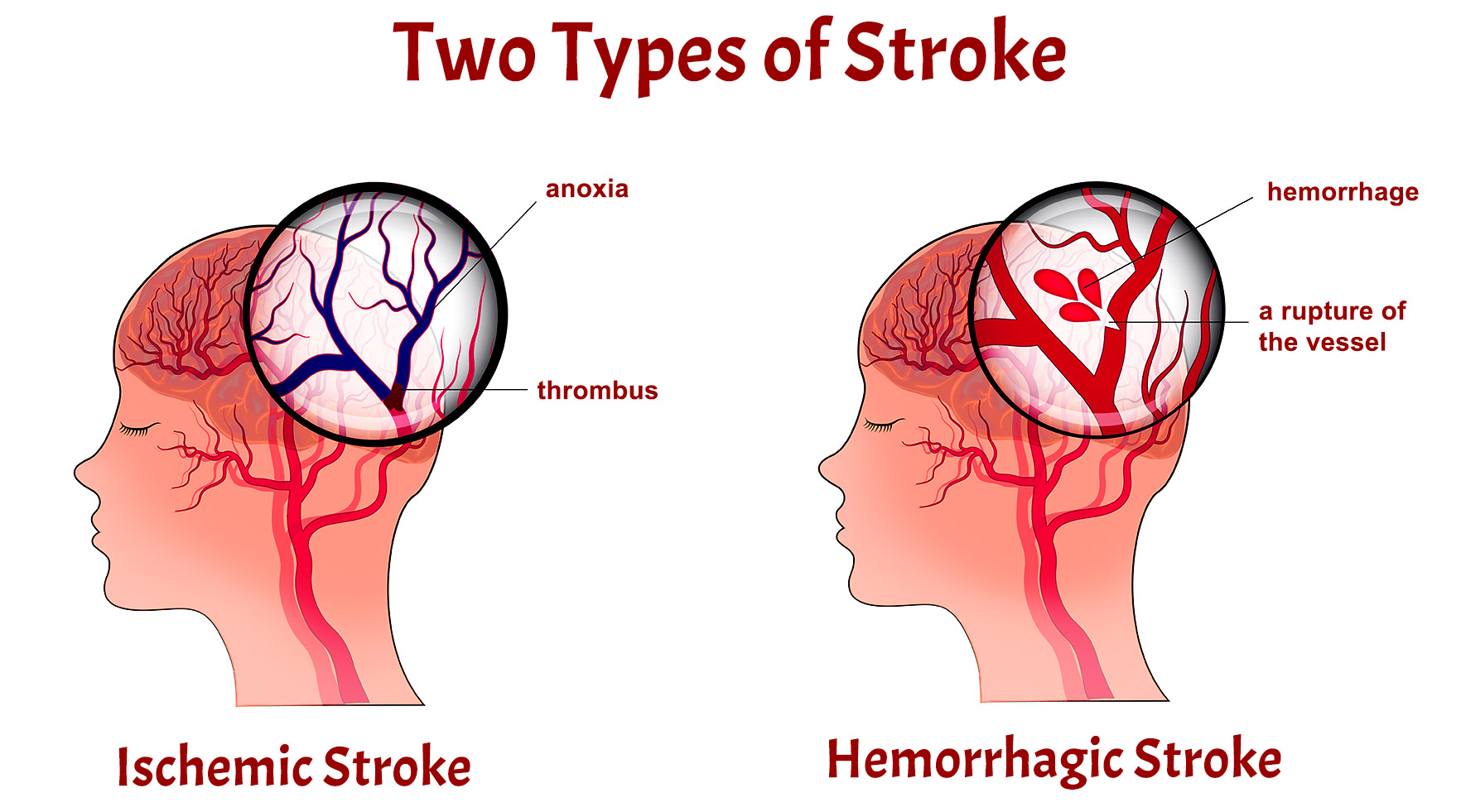
Antihypertensive therapy is crucial for managing hypertension (HTN), a significant risk factor for both ischemic and hemorrhagic strokes. Individuals with HTN experience increased shearing forces on the vascular endothelium, which can accelerate the development of atherosclerosis. Consequently, antihypertensive medications are prescribed to lower blood pressure and reduce the risk of stroke. Untreated HTN puts individuals at approximately four times greater risk of experiencing a cerebrovascular accident compared to those with normal blood pressure.
Toxic adenoma of the thyroid gland refers to a hyperfunctioning thyroid nodule that produces excess thyroid hormones, leading to hyperthyroidism. Common symptoms include weight loss, palpitations, heat intolerance, fatigue, and tachycardia. Laboratory findings typically show decreased levels of thyroid-stimulating hormone (TSH) and increased levels of free triiodothyronine (T3) and thyroxine (T4). Radioactive iodine (RAI) uptake studies reveal increased uptake in a single nodule, distinguishing it from other thyroid conditions such as subacute thyroiditis, Graves’ disease, and toxic multinodular goiter.
Penicillin is a commonly used antibiotic, but its use is not effective against the painless chancroid on the glans of the penis, which is characteristic of syphilis. Syphilis is a sexually transmitted infection caused by the bacterium Treponema pallidum. While penicillin remains the treatment of choice for syphilis, other antibiotics may be prescribed for individuals allergic to penicillin. It’s essential to accurately diagnose and treat syphilis to prevent the progression of the disease and its complications.
Pancreatic adenocarcinoma, a common type of pancreatic tumor, often presents with characteristic signs and symptoms. One notable manifestation is the compression and dilation of both the pancreatic duct and the common bile duct, referred to as the double duct sign. This compression can lead to elevated levels of alkaline phosphatase (ALP) and direct bilirubin. Additionally, unexplained migratory thrombophlebitis, a condition characterized by the development of blood clots in superficial veins that migrate from one location to another, is frequently observed in patients with pancreatic adenocarcinoma.
Beta-thalassemia trait results from a decrease in the synthesis of beta-globin chains, leading to an increased proportion of hemoglobin A2 (HbA2) relative to normal. This condition is often asymptomatic, with individuals typically experiencing mild or no clinical manifestations. Diagnosis is commonly made through laboratory tests revealing elevated levels of HbA2. Management usually involves monitoring for complications and providing genetic counseling to affected individuals and their families.
Tuberculosis is an infectious disease caused by the bacterium Mycobacterium tuberculosis. Common symptoms include fever, chills, and hemoptysis (coughing up blood). Reactivation tuberculosis, which occurs when dormant bacteria become active again, often affects the apices (upper regions) of the lungs. Diagnosis typically involves a combination of clinical evaluation, imaging studies, and microbiological testing, with treatment consisting of a multi-drug regimen aimed at eradicating the infection.
Catheterization of the bladder is a common medical procedure used to relieve bladder obstruction or distention. Patients with bladder obstruction often present with symptoms such as dysuria (painful urination) and a tender suprapubic mass due to the accumulation of urine. Catheterization is performed to drain the bladder and alleviate the obstruction, which can be caused by various factors such as prostate enlargement or neurogenic bladder dysfunction.
Complete heart block, also known as third-degree atrioventricular block, is a cardiac conduction disorder characterized by a lack of association between P waves and QRS complexes on an electrocardiogram (ECG). Additionally, the R-R interval remains regular despite the absence of a relationship between atrial and ventricular contractions. This condition can result in bradycardia and symptoms such as dizziness, syncope, or heart failure. Treatment options may include cardiac pacing to restore normal heart rhythm and prevent complications.
Hypomagnesemia refers to low levels of magnesium in the blood, which can have various causes including malnutrition, gastrointestinal disorders, or certain medications. Severe hypomagnesemia can suppress parathyroid hormone (PTH) secretion, leading to hypocalcemia (low blood calcium levels) due to impaired calcium absorption and bone mineralization. Chronic alcoholism is a common predisposing factor for hypomagnesemia due to decreased dietary intake, renal losses, and impaired gastrointestinal absorption of magnesium.
Adding simvastatin to a patient’s current regimen is indicated for individuals aged 40 to 75 with diabetes mellitus, as they are at increased risk of cardiovascular events. Simvastatin is a statin medication that works by inhibiting the enzyme HMG-CoA reductase, thereby reducing cholesterol production in the liver. Lowering cholesterol levels is crucial for preventing atherosclerosis and its complications, such as heart attacks and strokes, in diabetic patients who are already at elevated cardiovascular risk.
Hematogenous dissemination of distant infection can lead to conditions such as Pott disease, an extra-pulmonary form of tuberculosis. In this process, infectious agents spread through the bloodstream and seed distant sites in the body. In the case of Pott disease, hematogenous dissemination leads to infection of the vertebral bones, resulting in vertebral osteomyelitis. This infection can then spread contiguously to involve adjacent vertebrae and intervertebral discs, causing characteristic symptoms such as back pain and spinal deformities.
Adequate control of blood pressure is essential for preventing complications associated with hypertension (HTN), such as left ventricular hypertrophy (LVH) and reduced ejection fraction (EF). LVH is a common consequence of chronic high blood pressure and increases the risk of heart failure and arrhythmias. By effectively controlling blood pressure through lifestyle modifications and medications, further damage to the heart can be prevented, ultimately reducing the risk of cardiovascular events such as heart attacks and strokes.
Tracheomalacia is a condition characterized by the weakening of the supporting cartilage in the trachea, leading to collapse of the airway during expiration. This collapse can result in symptoms such as respiratory distress, wheezing, and difficulty breathing. Long-term intubation, particularly in critically ill patients, can contribute to tracheal weakening and structural damage to the tracheal cartilage, predisposing individuals to tracheomalacia. Management may involve supportive measures such as bronchodilators or, in severe cases, surgical interventions to stabilize the airway.
Cor pulmonale refers to the impaired function of the right ventricle (RV) due to pulmonary hypertension, which is defined by a pulmonary systolic pressure exceeding 25 mmHg. This condition often manifests with symptoms such as dyspnea, fatigue, and exertional angina, reflecting the decreased ability of the right heart to pump blood efficiently. Clinical signs of cor pulmonale include jugular venous distention (JVD), ascites, hepatomegaly, and pitting edema, indicative of fluid retention and right heart failure. Treatment strategies typically focus on managing the underlying cause of pulmonary hypertension, such as chronic obstructive pulmonary disease (COPD) or pulmonary embolism, and alleviating symptoms through medications like diuretics and oxygen therapy.
0.9% saline, or isotonic saline, is commonly administered intravenously prior to contrast-enhanced computed tomography (CT) scans to prevent contrast-induced nephropathy. This balanced saline solution helps restore renal perfusion and maintain adequate hydration, reducing the risk of kidney injury associated with contrast media administration. By expanding intravascular volume, isotonic saline promotes renal blood flow and dilutes the contrast agent, mitigating its nephrotoxic effects. This preventive measure is especially crucial for patients with preexisting renal impairment or risk factors for contrast-induced nephropathy, ensuring the safety and efficacy of contrast-enhanced imaging procedures.
Nephrogenic diabetes insipidus (NDI) is a renal disorder characterized by the kidney’s inability to respond to antidiuretic hormone (ADH), resulting in excessive urine production and consequent dehydration. Hypercalcemia can induce nephron damage, leading to the development of NDI and its associated symptoms, including polyuria, polydipsia, and volume depletion. Unlike central diabetes insipidus, which involves inadequate ADH secretion, nephrogenic DI arises from defects in the renal tubules, impairing the reabsorption of water. Management strategies for NDI focus on addressing the underlying cause of renal dysfunction and may include dietary modifications, medications, and fluid replacement therapy to prevent dehydration and electrolyte imbalances.
Crohn’s disease is a chronic inflammatory bowel disease characterized by recurring episodes of abdominal pain, diarrhea, weight loss, and evidence of intestinal inflammation. This condition can affect any part of the gastrointestinal tract, from the mouth to the anus, and often presents with non-specific symptoms such as fatigue and malaise. Diagnosis typically involves a combination of clinical evaluation, imaging studies, endoscopic procedures, and histological examination of tissue samples. Treatment strategies for Crohn’s disease aim to reduce inflammation, alleviate symptoms, and prevent complications through medications, dietary modifications, and in some cases, surgical interventions to remove diseased bowel segments.
Hot tub use has been associated with a form of hypersensitivity pneumonitis known as “hot tub lung,” caused by exposure to aerosolized Mycobacterium avium complex (MAC) bacteria. Inhalation of these bacteria, commonly found in contaminated hot tub water, can trigger an inflammatory response in the lungs, leading to symptoms such as cough, dyspnea, and constitutional symptoms resembling flu-like illness. Diagnosis of hot tub lung typically involves clinical evaluation, imaging studies, pulmonary function tests, and exclusion of other respiratory conditions. Management often entails discontinuation of hot tub use, avoidance of environmental triggers, and treatment with corticosteroids to alleviate inflammation and respiratory symptoms.
Adding fluticasone, an inhaled corticosteroid (ICS), is recommended for patients with mild persistent asthma to improve asthma control and reduce the risk of exacerbations. Inhaled corticosteroids work by reducing airway inflammation and hyperresponsiveness, thereby preventing asthma symptoms and improving lung function over time. Fluticasone is often prescribed in combination with a short-acting beta agonist (SABA) such as albuterol for symptom relief as needed. This step-up therapy is part of a stepwise approach outlined in asthma management guidelines, which aim to achieve and maintain asthma control through regular assessment and adjustment of treatment based on disease severity and patient response.
Lymphangitis refers to the inflammation of lymphatic channels, commonly occurring as a result of infection or trauma at a site distal to the affected lymphatics. This condition typically presents with visible red streaks along the course of the inflamed lymphatic vessels, known as lymphangitic streaks. Infection-induced lymphangitis is often associated with symptoms such as fever, local tenderness, and regional lymphadenopathy, accompanied by systemic signs of inflammation such as leukocytosis and a left shift in white blood cell count. Prompt diagnosis and treatment of the underlying infection are crucial to prevent complications such as abscess formation or systemic spread of infection.
Serum anti-mitochondrial antibody assays are used in the diagnosis of primary biliary cholangitis (PBC), a chronic autoimmune liver disease characterized by immune-mediated destruction of small bile ducts within the liver. Patients with PBC typically present with elevated levels of anti-mitochondrial antibodies (AMA), particularly in middle-aged women. This serologic marker, along with a cholestatic pattern of liver injury characterized by elevated alkaline phosphatase (ALP), aspartate aminotransferase (AST), and alanine aminotransferase (ALT) levels, helps distinguish PBC from other liver disorders. Common symptoms of PBC include fatigue, pruritus, and hepatomegaly, although the disease can remain asymptomatic in some individuals.
A computed tomography (CT) scan of the abdomen may be indicated to evaluate adrenal function and visualize adrenal tumors secreting dehydroepiandrosterone sulfate (DHEAS). Increased levels of DHEAS, a precursor of adrenal androgens, along with the absence of cortisol suppression after overnight dexamethasone administration, suggest an adrenal origin for hyperandrogenism. Adrenal imaging helps localize the source of hormone overproduction, guiding further diagnostic and therapeutic interventions. In cases of adrenal tumors, surgical resection may be warranted to alleviate symptoms and prevent complications associated with excess adrenal hormone secretion.
Alendronate is a bisphosphonate medication commonly used for the long-term treatment of osteoporosis, a condition characterized by reduced bone density and increased fracture risk. Bisphosphonates exert their therapeutic effects by inhibiting osteoclast activity, thereby slowing down bone resorption and preserving bone mass. In addition to pharmacological interventions, management of osteoporosis typically includes calcium and vitamin D supplementation, along with lifestyle modifications such as regular weight-bearing exercise and smoking cessation. Regular monitoring of bone mineral density and adherence to treatment regimens are essential for optimizing outcomes and reducing the risk of fractures in individuals with osteoporosis.
Nitrofurantoin therapy is commonly used for the treatment of uncomplicated cystitis, along with other antibiotics such as trimethoprim-sulfamethoxazole (TMP-SMX) or fosfomycin. Nitrofurantoin exerts its antimicrobial effects primarily in the urinary tract, making it a preferred choice for urinary tract infections. However, its efficacy may be limited by increasing rates of bacterial resistance. Common adverse effects of nitrofurantoin therapy include gastrointestinal symptoms such as nausea and diarrhea, as well as less commonly, pulmonary reactions such as acute pneumonitis. Monitoring for adverse effects and ensuring appropriate dosing are essential components of nitrofurantoin therapy to optimize clinical outcomes and minimize risks.
Acute respiratory distress syndrome (ARDS) is a life-threatening condition characterized by non-cardiogenic lung injury leading to inflammation and the accumulation of fluid in the alveoli, impairing gas exchange. Radiographic findings typically show bilateral lung opacities on chest X-ray, reflecting diffuse alveolar damage. Trauma, including intubation-related lung injury, is a common risk factor for ARDS, along with sepsis, pneumonia, and aspiration. Hypoxemia, often refractory to supplemental oxygen therapy, is a hallmark feature of ARDS, with a PaO2/FiO2 ratio less than 300 mmHg indicating severe impairment of gas exchange. Management involves supportive care, including mechanical ventilation with low tidal volumes and positive end-expiratory pressure (PEEP), along with addressing the underlying cause of lung injury.
Pulmonary contusion typically presents within 24 hours following blunt thoracic trauma, characterized by injury to the underlying lung parenchyma leading to alveolar hemorrhage and impaired gas exchange. Clinical manifestations include tachypnea, tachycardia, and hypoxia, often accompanied by chest pain and hemoptysis. Chest X-ray findings may reveal patchy, non-segmental areas of consolidation reflecting alveolar infiltrates not confined by anatomical borders. Management focuses on supportive care, including pain control, supplemental oxygen therapy, and close monitoring for complications such as pneumonia and respiratory failure. Severe cases may require mechanical ventilation and surgical intervention for complications such as pulmonary hemorrhage or pneumothorax.
Small cell carcinoma of the lung is a highly aggressive subtype of lung cancer strongly associated with smoking. Small cell lung cancer often presents with paraneoplastic syndromes, including Cushing syndrome due to ectopic adrenocorticotropic hormone (ACTH) production, syndrome of inappropriate antidiuretic hormone (SIADH) secretion, and Lambert-Eaton myasthenic syndrome (LEMS) caused by antibodies against presynaptic voltage-gated calcium channels. Diagnosis typically involves histological examination of tissue samples obtained via bronchoscopy or biopsy, along with staging studies to determine the extent of disease spread. Treatment options for small cell lung cancer include chemotherapy, radiation therapy, and immunotherapy, with prognosis generally poor due to the aggressive nature of the disease and high rates of metastasis.
Necrotizing otitis externa is a potentially life-threatening infection of the external auditory canal typically seen in elderly individuals, particularly those with diabetes mellitus. Risk factors include advanced age, diabetes mellitus, and a history of aural irrigation. Clinical manifestations include severe ear pain, otorrhea, and granulation tissue within the external auditory canal, often accompanied by elevated erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) levels. Prompt diagnosis and aggressive treatment with broad-spectrum antibiotics, along with management of underlying risk factors such as glycemic control in diabetic patients, are essential to prevent complications such as skull base osteomyelitis and cranial nerve palsies.
Decreased absorption due to decreased serum 1,25-dihydroxycholecalciferol concentration occurs in conditions such as renal failure, where the kidney’s ability to convert 25-hydroxycholecalciferol (inactive vitamin D) to its active form, 1,25-dihydroxycholecalciferol, is impaired. This active form of vitamin D plays a crucial role in regulating calcium absorption in the intestines and promoting renal reabsorption of calcium. In renal failure, the decreased production of active vitamin D leads to reduced calcium absorption in the gut, contributing to hypocalcemia and secondary hyperparathyroidism. Management often involves supplementation with active vitamin D analogs or calcitriol to maintain calcium and phosphorus homeostasis in patients with renal insufficiency.
Uremia, a clinical syndrome resulting from the accumulation of uremic toxins in the bloodstream due to renal failure, can lead to various systemic manifestations, including pericarditis. In the setting of acute or chronic renal failure, elevated blood urea nitrogen (BUN) levels can lead to inflammation of the pericardial layers, resulting in pericarditis. Common clinical findings in uremic pericarditis include friction rub and substernal chest pain, which can be exacerbated by respiratory movements and relieved by leaning forward. Diagnosis is based on clinical evaluation, along with laboratory tests demonstrating elevated BUN levels (>60 mg/dL) and signs of pericardial inflammation on electrocardiogram (ECG) or echocardiography. Management typically involves addressing the underlying cause of uremia, along with symptomatic treatment of pericarditis using nonsteroidal anti-inflammatory drugs (NSAIDs) or colchicine.
IgA nephropathy, also known as Berger’s disease, is a primary glomerulonephritis characterized by the deposition of IgA antibodies within the glomerular mesangium, leading to recurrent episodes of gross hematuria, often following upper respiratory tract infections (URTI). This condition is more commonly observed in men aged 20-30 and may present with episodes of hematuria, proteinuria, and occasionally, renal insufficiency. Diagnosis is typically confirmed by renal biopsy, which reveals mesangial proliferation and deposition of IgA on immunofluorescence staining. Management involves supportive measures such as blood pressure control and renin-angiotensin system blockade to delay disease progression and minimize proteinuria.
Quantitative serum immunoglobulin testing plays a crucial role in the diagnosis of common variable immunodeficiency (CVID), a primary immunodeficiency disorder characterized by impaired B cell differentiation and hypogammaglobulinemia. Patients with CVID commonly present with recurrent respiratory and gastrointestinal infections, including sinusitis, otitis, pneumonia, and enteritis, caused by opportunistic pathogens such as Salmonella and Campylobacter. Laboratory findings typically reveal decreased levels of serum immunoglobulins, particularly IgG, IgA, and IgM, indicating defective antibody production. Treatment involves lifelong immunoglobulin replacement therapy to prevent infections and reduce the risk of complications such as bronchiectasis and autoimmune diseases.
Acetaminophen is commonly used to manage febrile non-hemolytic transfusion reactions, the most common adverse reactions occurring within 1-6 hours of blood transfusion. These reactions are characterized by fever, chills, and malaise without evidence of hemolysis or other transfusion-related complications. Acetaminophen effectively alleviates symptoms associated with febrile reactions by reducing fever and discomfort. However, it is essential to monitor patients for signs of more severe transfusion reactions, such as acute hemolytic reactions or transfusion-related acute lung injury (TRALI), which may require prompt intervention and discontinuation of transfusion.
Heat stroke, a severe form of heat-related illness, can occur due to prolonged exposure to hot and humid conditions, particularly in individuals with advanced age who may have difficulty regulating body temperature or obtaining adequate fluids. Non-exertional heat stroke often occurs in vulnerable populations such as the elderly, infants, and individuals with certain medical conditions. It is characterized by a core body temperature exceeding 40 degrees Celsius (104 degrees Fahrenheit), accompanied by central nervous system dysfunction and additional organ damage. Prompt recognition and treatment are essential to prevent complications such as heat-related organ failure and death, with management focusing on rapid cooling, hydration, and supportive care.
Increased creatine kinase (CK) activity in serum is commonly observed in conditions such as rhabdomyolysis, where skeletal muscle breakdown leads to the release of CK into the bloodstream. Rhabdomyolysis can occur due to various causes, including prolonged immobilization, trauma, medications, and metabolic disorders. Serum studies typically reveal markedly elevated CK levels (>1,000 U/L), along with abnormalities in electrolytes such as hyperkalemia, hyperphosphatemia, and hypocalcemia. Additionally, liver enzymes such as aspartate aminotransferase (AST) and alanine aminotransferase (ALT) may also be elevated, reflecting muscle damage and hepatocellular injury. Management of rhabdomyolysis involves fluid resuscitation, electrolyte monitoring, and addressing the underlying cause to prevent complications such as acute kidney injury and compartment syndrome.
Immediate groin exploration is indicated in cases of suspected incarcerated inguinal hernia, a potentially serious condition where abdominal contents become trapped within the inguinal canal. Inguinal hernias commonly present with a visible bulge or mass in the groin area, often accompanied by pain and discomfort. In cases of incarceration, prompt surgical intervention is necessary to relieve the obstruction and prevent complications such as strangulation, ischemia, and bowel perforation. Groin exploration allows for direct visualization of the hernia sac and its contents, facilitating reduction of the herniated tissue and repair of the hernia defect. Delayed treatment of incarcerated hernias can lead to bowel necrosis, sepsis, and life-threatening complications requiring emergent surgery.
Spinal cord involvement in multiple sclerosis (MS) often presents with neurological deficits disseminated in space and time, suggesting demyelinating lesions affecting various areas of the central nervous system. Transverse myelitis, a common manifestation of MS, is characterized by motor and sensory loss below the level of the lesion, along with bowel and bladder dysfunction. Patients may initially experience flaccid paralysis due to spinal shock, followed by spastic paralysis with hyperreflexia as the condition progresses. Diagnosis of MS involves clinical evaluation, neuroimaging studies such as magnetic resonance imaging (MRI), and analysis of cerebrospinal fluid for the presence of oligoclonal bands. Management focuses on disease-modifying therapies to reduce relapses and slow disease progression, along with symptomatic treatment to alleviate symptoms such as spasticity and neuropathic pain.
Magnetic resonance angiography (MRA) of the renal arteries is a valuable diagnostic tool for evaluating renovascular diseases such as renal artery stenosis (RAS), a common cause of secondary hypertension. Clinical manifestations of RAS may include resistant hypertension, malignant hypertension, or the onset of severe hypertension after the age of 55. Laboratory findings, such as an unexplained rise in serum creatinine levels (>30%) after starting angiotensin-converting enzyme (ACE) inhibitors, may also raise suspicion for RAS. MRA allows for non-invasive imaging of the renal arteries, providing detailed anatomical information about the degree and location of stenosis. Diagnosis of RAS via MRA facilitates appropriate management decisions, including medical therapy, endovascular interventions such as angioplasty and stenting, or surgical revascularization to improve blood flow to the kidneys and control hypertension.
Renal tubular acidosis (RTA) is a renal disorder characterized by impaired acid excretion, leading to a normal anion gap metabolic acidosis. Different types of RTA exist, with type I RTA, often associated with autoimmune conditions like rheumatoid arthritis (RA), characterized by an elevated urine pH due to impaired distal tubular acid secretion. On the other hand, type IV RTA, associated with conditions such as hyperkalemia and the use of medications like ACE inhibitors, manifests with a low urine pH. Diagnosis involves evaluating urinary electrolytes and pH, along with serum electrolyte levels. Treatment aims to correct acidosis and electrolyte imbalances, often involving alkali supplementation and addressing underlying causes such as autoimmune diseases or medication adjustments.
Surgical excision is the primary treatment modality for melanoma, a malignant skin neoplasm arising from melanocytes. The goal of surgical excision is to completely remove the tumor along with a margin of surrounding healthy tissue to minimize the risk of recurrence and metastasis. The extent of surgical excision depends on various factors, including the thickness and location of the melanoma, as well as the presence of ulceration or lymph node involvement. Additionally, sentinel lymph node biopsy may be performed to assess the spread of melanoma cells to regional lymph nodes. Adjuvant therapies such as immunotherapy or targeted therapy may be considered in certain cases to reduce the risk of recurrence or treat metastatic disease.
Following the advance directive is crucial in medical decision-making, as it legally documents a patient’s preferences regarding medical treatments and end-of-life care. An advance directive takes precedence over decisions made by next of kin or healthcare providers, ensuring that the patient’s wishes are respected even if they become incapacitated. Advance directives commonly include a living will, which outlines specific medical interventions a patient wishes to receive or avoid, and a healthcare proxy or durable power of attorney for healthcare, designating a trusted individual to make medical decisions on behalf of the patient if they are unable to do so themselves. Healthcare providers are obligated to adhere to the directives outlined in the advance directive, respecting the patient’s autonomy and dignity in medical decision-making.
HIV infection with candidal esophagitis is a common opportunistic infection seen in patients with advanced HIV disease. Acute HIV infection typically presents 2-4 weeks after exposure with symptoms such as fever, lymphadenopathy, sore throat, and rash, resembling a mononucleosis-like syndrome. Candidal esophagitis, characterized by dysphagia, odynophagia, and white plaques in the buccal mucosa, is a common manifestation of HIV-related immunosuppression. Diagnosis involves endoscopic evaluation with biopsy and fungal culture, along with HIV testing. Treatment of candidal esophagitis typically involves antifungal therapy such as fluconazole or oral nystatin, along with antiretroviral therapy to control HIV replication and improve immune function.
Glucocorticoid therapy is the first-line treatment for symptomatic sarcoidosis, a systemic granulomatous disorder that commonly affects African Americans. Sarcoidosis can present with various symptoms, including cough, dyspnea, chest pain, hypercalcemia, and bilateral hilar adenopathy or pulmonary reticular infiltrates on imaging studies. Glucocorticoids, such as prednisone, suppress inflammation and immune responses, helping to reduce granuloma formation and alleviate symptoms. Treatment duration and dosing vary depending on the extent and severity of organ involvement, with close monitoring for side effects such as immunosuppression, osteoporosis, and hyperglycemia. In refractory cases or those intolerant to glucocorticoids, immunomodulatory agents such as methotrexate or TNF-alpha inhibitors may be considered as alternative therapies.
Oral acyclovir is the first-line treatment for herpetic whitlow, a viral infection characterized by painful vesicular lesions on the fingers caused by herpes simplex virus (HSV) infection. Acyclovir, an antiviral medication, works by inhibiting viral DNA replication, thereby reducing the severity and duration of symptoms associated with HSV infections. Treatment with oral acyclovir should be initiated promptly upon diagnosis of herpetic whitlow to expedite symptom resolution and prevent complications such as secondary bacterial infection or dissemination of the virus. The recommended dosage and duration of acyclovir therapy may vary depending on the severity of the infection and the patient’s immune status, with some cases requiring intravenous acyclovir for severe or disseminated disease. Additionally, topical antiviral creams or ointments may be used adjunctively to alleviate discomfort and promote lesion healing.
Obesity poses a significant risk factor for the development of osteoarthritis (OA), a degenerative joint disease characterized by the breakdown of cartilage and subsequent joint pain and dysfunction. Excessive body weight places increased stress on weight-bearing joints such as the knees, hips, and spine, accelerating the degenerative changes associated with OA. Chronic mechanical overload and inflammation in obese individuals contribute to cartilage damage, synovial inflammation, and alterations in joint biomechanics, predisposing them to the development and progression of OA. Management of obesity is crucial in reducing the risk of OA and improving joint health, with interventions such as weight loss, exercise, and dietary modifications aimed at reducing excess body weight and alleviating joint strain. Additionally, pharmacological therapies, physical therapy, and surgical interventions may be considered to manage symptoms and improve functional outcomes in individuals with obesity-related OA.
Exposure to nickel is a common cause of contact dermatitis, an inflammatory skin condition characterized by erythema, pruritus, and vesicular or bullous lesions at the site of contact with the allergen. Nickel, a ubiquitous metal found in various consumer products such as jewelry, clothing fasteners, and electronic devices, is one of the most common allergens responsible for allergic contact dermatitis worldwide. Sensitization to nickel typically occurs through repeated or prolonged exposure to nickel-containing items, leading to the development of delayed hypersensitivity reactions upon subsequent contact. Diagnosis of nickel-induced contact dermatitis involves patch testing with a standard series of allergens, including nickel sulfate, to confirm hypersensitivity. Management focuses on identifying and avoiding sources of nickel exposure, along with symptomatic relief using topical corticosteroids, emollients, and antihistamines to alleviate inflammation and pruritus associated with allergic reactions.
Ruptured congenital aneurysm is a potentially life-threatening medical emergency characterized by sudden onset severe headache, often described as the “worst headache of my life,” accompanied by neurological symptoms such as altered mental status, focal deficits, or loss of consciousness. Subarachnoid hemorrhage (SAH) accounts for the majority of cases of ruptured congenital aneurysms, with bleeding into the subarachnoid space resulting from the rupture of intracranial aneurysms, most commonly located at the branching points of the Circle of Willis. Prompt recognition and management of SAH are essential to prevent complications such as cerebral vasospasm, rebleeding, and neurological deficits. Diagnosis of SAH involves neuroimaging studies such as computed tomography (CT) or magnetic resonance imaging (MRI) of the brain, along with cerebrospinal fluid analysis to confirm the presence of blood in the subarachnoid space. Treatment strategies for ruptured congenital aneurysms may include neurosurgical clipping or endovascular coiling to prevent rebleeding and minimize the risk of neurological sequelae.
Phlebotomy is the first-line treatment for polycythemia vera (PV), a myeloproliferative disorder characterized by the clonal proliferation of erythrocytes, leukocytes, and platelets. PV results in an increase in blood viscosity due to elevated red blood cell mass, leading to symptoms such as hypertension, erythromelalgia (burning pain and cyanosis in the hands and feet), transient visual disturbances, and aquagenic pruritus. Diagnosis of PV involves laboratory evaluation showing increased hemoglobin, leukocyte, and platelet counts, along with decreased erythropoietin (EPO) levels. Phlebotomy, the removal of excess blood, is the cornerstone of treatment for PV, aimed at reducing blood viscosity and the risk of thrombotic complications such as stroke or myocardial infarction. Additionally, cytoreductive therapy with medications such as hydroxyurea or interferon-alpha may be considered to suppress bone marrow activity and maintain hematologic parameters within target ranges. Regular monitoring and individualized management are essential to optimize outcomes and minimize the risk of thrombotic or hemorrhagic events in patients with PV.
Check out the answers and explanations for NBME internal medicine Form 6 practice exam here and NBME internal medicine Form 4.
Check out these popular articles
Circulatory System: Blood Flow Pathway Through the Heart
Ectoderm vs Endoderm vs Mesoderm
Circulatory System: Heart Structures and Functions
Ductus Arteriosus Vs Ductus Venosus Vs Foramen Ovale: Fetal Heart Circulation
Autocrine vs Paracrine vs Endocrine: What are the Differences?
Upper Vs Lower Respiratory System: Upper vs Lower Respiratory Tract Infections
Seven General Functions of the Respiratory System
Kidney Embryology & Development: Easy Lesson
Psychology 101: Crowd Psychology and The Theory of Gustave Le Bon
Cell Membrane Dynamics: Flippase Vs Floppase Vs Scramblase
Shoulder Abduction Muscles: Medical Anatomy and USMLE
Top Websites Like Sparknotes: 15 Free Sites and Resources Similar to Sparknotes
Cell Membrane Fluidity: Factors That Influence and Increase the Cell Membrane Fluidity
NBME 4, NBME 5, NBME 6 Internal Medicine Forms Answers and Explanations
Copyright © 2024 Moosmosis Organization: All Rights Reserved
All rights reserved. This essay first published on moosmosis.org or any portion thereof may not be reproduced or used in any manner whatsoever
without the express written permission of the publisher at moosmosis.org.
Please Like and Subscribe for free to our Email List at moosmosis.org to support our open-access youth education initiatives!
Hello friends! Here are notes and detailed explanations for questions and answers to the NBME internal medicine Form 5 practice exam. Hope this helps and good luck! Check out the answers and explanations for NBME internal medicine Form 4 and Form 6 practice exam here. anatomy, Biology, cell biology, education, health, medicine, stem, technology, anemia, autonomic nervous system, bleeding, brain, brain bleed, brain stem, brain surgery, cardiologist, cardiology, central nervous system, cerebellum, cerebrum, college, ct head, ECG, epidural hematoma, gray matter, heart attack, heart failure, hemorrhage, hemorrhagic stroke, internal medicine, interventional radiology, ischemic stroke, life, mcat, medical, medical student, MRI, MRI brain, NBME Form 4, NBME Form 6, nerves, neurology, neuron, neuroradiology, neuroscience, neurosurgery, NMBE medicine, parasympathetic, peripheral nervous system, physiology, pre-medical, radiology, reflex, resident, school, science, somatosensory, STEP exam, stretch reflex, stroke, student, subarachnoid hemorrhage, subcortical cerebrum, subdural hematoma, surgery, sympathetic, TIA, transient ischemic attack, university, upper motor neuron, white matter Moosmosis