Hey there, my friends! In this lesson, we explore pericarditis and cardiac tamponade which are two distinct cardiac conditions that can affect the pericardium, the sac-like structure surrounding the heart. While both conditions involve inflammation or fluid accumulation around the heart, they differ in their etiology, symptoms, diagnosis, treatment, and prognosis.
Pericarditis vs Cardiac Tamponade: Symptoms
Pericarditis Symptoms:
Pericarditis is characterized by inflammation of the pericardium, the double-layered sac that surrounds and protects the heart. The symptoms of pericarditis can vary widely in severity and duration but often include:
Chest Pain:
Chest pain is the hallmark symptom of pericarditis and is typically described as sharp, stabbing, or pressure-like.
The pain may be pleuritic, meaning it worsens with deep breathing, coughing, or changes in body position.
It may radiate to the neck, shoulders, back, or arms and is often relieved by sitting up and leaning forward.
Fever:
Many patients with pericarditis experience low-grade fever, although high fever may occur in cases of infectious pericarditis.
Dyspnea:
Shortness of breath or dyspnea may occur, particularly with exertion or in the setting of significant pericardial effusion.
Pericardial Friction Rub:
A pericardial friction rub, a scratching or grating sound heard on auscultation of the heart, may be present and is characteristic of pericarditis. However, it is not always present and may come and go.
Other Systemic Symptoms:
Patients with pericarditis may experience fatigue, malaise, and generalized weakness, though these symptoms are nonspecific and can occur in various conditions.
Cardiac Tamponade Symptoms:
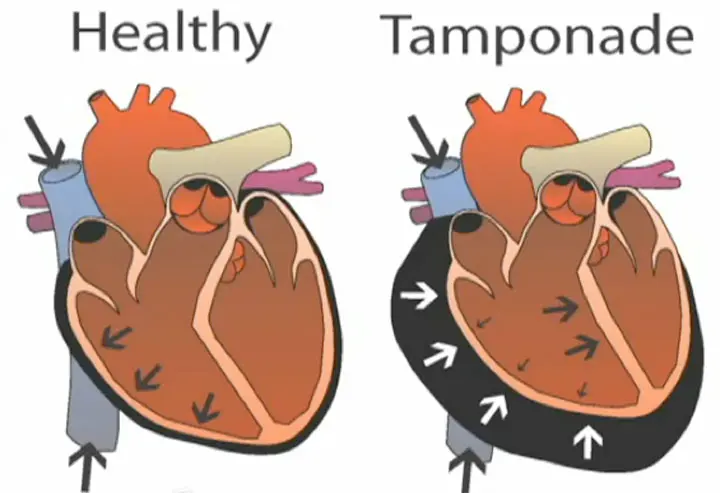
Cardiac tamponade is a medical emergency resulting from the accumulation of fluid or blood in the pericardial sac, leading to increased pressure on the heart and impaired cardiac function. The symptoms of cardiac tamponade typically develop rapidly and may include:
Beck’s Triad:
Beck’s triad consists of three classic signs: hypotension (low blood pressure), distended neck veins (jugular venous distension), and muffled heart sounds.
Hypotension occurs due to decreased cardiac output as a result of impaired ventricular filling.
Distended neck veins result from increased pressure in the superior vena cava due to impaired right heart filling.
Muffled heart sounds occur because the fluid in the pericardial sac dampens the transmission of heart sounds to the chest wall.
Pulsus Paradoxus:
Pulsus paradoxus refers to an exaggerated drop in systolic blood pressure (>10 mmHg) during inspiration.
It occurs because the increased intrathoracic pressure during inspiration further compresses the heart within the rigid pericardial sac, leading to decreased cardiac output.
Dyspnea and Tachycardia:
Patients with cardiac tamponade may experience dyspnea (shortness of breath) and tachycardia (rapid heart rate) due to decreased cardiac output and compensatory mechanisms.
Other Symptoms:
Other symptoms may include weakness, fatigue, anxiety, confusion, and altered mental status, which can result from decreased cerebral perfusion due to impaired cardiac output.
Pericarditis vs Cardiac Tamponade: Diagnosis
Pericarditis Diagnosis:
Diagnosing pericarditis typically involves a combination of clinical evaluation, medical history, physical examination, and diagnostic tests. Key steps in the diagnostic process include:
Clinical Evaluation:
A thorough assessment of the patient’s medical history, including risk factors for pericarditis such as recent viral illness, autoimmune disease, or myocardial infarction, provides valuable diagnostic clues.
Inquiring about symptoms such as chest pain, fever, dyspnea, and fatigue helps in identifying characteristic features of pericarditis.
Physical Examination:
A physical examination may reveal findings consistent with pericarditis, including pericardial friction rub, which is a scratching or grating sound heard over the precordium with each heartbeat.
Other signs such as tachycardia, fever, and evidence of underlying conditions (e.g., pleural effusion in connective tissue diseases) may also be present.
Electrocardiography (ECG):
Electrocardiography plays a crucial role in diagnosing pericarditis by revealing characteristic ECG changes, including diffuse ST-segment elevation and PR-segment depression.
These changes, known as the “pericarditis pattern,” are typically seen in multiple leads and are transient, resolving as the inflammation resolves.
Echocardiography:
Echocardiography is a valuable imaging modality for assessing pericardial effusion and evaluating cardiac function.
It can detect the presence and size of pericardial effusion, as well as assess for complications such as cardiac tamponade or constrictive pericarditis.
Cardiac Tamponade Diagnosis:
Diagnosing cardiac tamponade requires prompt recognition of clinical signs and symptoms, followed by confirmatory diagnostic tests. Key steps in the diagnostic process include:
Clinical Evaluation:
A high index of suspicion for cardiac tamponade is necessary in patients presenting with symptoms such as hypotension, distended neck veins, and muffled heart sounds (Beck’s triad).
Additional symptoms such as dyspnea, tachycardia, pulsus paradoxus, weakness, and altered mental status may also be present.
Physical Examination:
A physical examination may reveal classic findings of cardiac tamponade, including hypotension, distended neck veins, and muffled heart sounds.
Pulsus paradoxus, defined as an exaggerated drop in systolic blood pressure (>10 mmHg) during inspiration, is a hallmark sign of cardiac tamponade.
Echocardiography:
Echocardiography is the primary imaging modality for diagnosing cardiac tamponade and assessing its severity.
It can visualize pericardial effusion, quantify its size, and evaluate its hemodynamic significance by assessing cardiac chamber collapse during diastole.
Other Diagnostic Tests:
Additional tests such as chest X-ray and computed tomography (CT) scan may be performed to evaluate the underlying cause of pericardial effusion and assess for signs of hemodynamic compromise.
Chest X-Ray with Marked Cardiomegaly due to Cardiac Tamponade
Pericarditis vs Cardiac Tamponade: Treatment
Pericarditis Treatment:
The treatment of pericarditis aims to reduce inflammation, alleviate symptoms, and prevent recurrence. Key components of pericarditis management include:
Nonsteroidal Anti-inflammatory Drugs (NSAIDs):
NSAIDs, such as ibuprofen or aspirin, are often used as first-line therapy to reduce inflammation and alleviate chest pain in acute pericarditis.
These medications inhibit prostaglandin synthesis, thereby reducing pericardial inflammation and pain.
Colchicine:
Colchicine is an anti-inflammatory medication that may be used as adjunctive therapy in cases of recurrent or refractory pericarditis.
It inhibits the inflammatory response and can help prevent recurrence by suppressing the release of inflammatory mediators.
Corticosteroids:
Corticosteroids may be considered in cases of severe or recurrent pericarditis, particularly if NSAIDs and colchicine are ineffective or contraindicated.
However, corticosteroids are generally reserved for specific situations due to the risk of side effects and potential for masking underlying infections.
Management of Underlying Causes:
Identifying and treating underlying causes of pericarditis, such as viral or bacterial infections, autoimmune diseases, or myocardial infarction, is essential for preventing recurrence.
Cardiac Tamponade Treatment:
The treatment of cardiac tamponade is focused on relieving pericardial pressure, restoring cardiac function, and stabilizing the patient’s hemodynamic status. Key components of cardiac tamponade management include:
Pericardiocentesis:
Pericardiocentesis, a procedure to drain fluid from the pericardial sac, is the primary treatment for cardiac tamponade.
It involves inserting a needle or catheter into the pericardial space under ultrasound or fluoroscopic guidance to remove excess fluid and relieve cardiac compression.
Volume Expansion:
In cases of hemodynamic instability, volume expansion with intravenous fluids may be necessary to improve cardiac output and blood pressure.
However, cautious fluid administration is essential to avoid exacerbating pericardial effusion and worsening tamponade.
Surgical Interventions:
In cases of recurrent or chronic tamponade, or when pericardiocentesis is not feasible or successful, surgical interventions such as pericardial window or pericardiectomy may be considered.
These procedures involve creating a permanent opening in the pericardium to allow continuous drainage of pericardial fluid and prevent recurrence of tamponade.
Treatment of Underlying Causes:
Identifying and treating the underlying cause of pericardial effusion, such as malignancy, infection, or autoimmune disease, is crucial for preventing recurrence and optimizing long-term outcomes.
Pericarditis vs Cardiac Tamponade: Prognosis
Pericarditis Prognosis:
The prognosis of pericarditis is generally favorable, with most patients experiencing resolution of symptoms and a low risk of complications. However, the prognosis may vary depending on several factors, including:
Underlying Cause:
The prognosis of pericarditis is influenced by the underlying cause. Pericarditis secondary to viral or idiopathic etiology often resolves spontaneously with appropriate treatment, whereas pericarditis associated with conditions such as malignancy or autoimmune diseases may have a more variable course.
Recurrence:
Recurrent pericarditis is common and may occur in up to 15-30% of cases, particularly in patients with idiopathic or viral pericarditis.
Recurrences are typically milder and may respond to reinitiation or adjustment of anti-inflammatory therapy.
Complications:
While pericarditis itself is usually benign, complications such as pericardial effusion, cardiac tamponade, and constrictive pericarditis may occur and impact prognosis.
Complications are more common in cases of bacterial or tuberculous pericarditis and may require additional interventions or surgical management.
Response to Treatment:
The prognosis of pericarditis is generally favorable with appropriate treatment, including nonsteroidal anti-inflammatory drugs (NSAIDs), colchicine, and corticosteroids.
Most patients experience resolution of symptoms within a few weeks to months, with a low risk of long-term sequelae.
Cardiac Tamponade Prognosis:
Cardiac tamponade is a life-threatening condition requiring prompt recognition and intervention to prevent hemodynamic collapse and death. The prognosis of cardiac tamponade depends on several factors, including:
Timeliness of Treatment:
Early recognition and prompt intervention are crucial for improving outcomes in cardiac tamponade.
Delayed diagnosis or treatment may result in hemodynamic instability, cardiogenic shock, and death.
Severity of Hemodynamic Compromise:
The severity of cardiac tamponade, as indicated by the degree of hemodynamic compromise and symptoms such as hypotension and pulsus paradoxus, influences prognosis.
Patients with profound hemodynamic instability or shock have a higher risk of morbidity and mortality.
Underlying Cause:
Identifying and treating the underlying cause of cardiac tamponade, such as malignancy, infection, or trauma, is essential for optimizing outcomes.
Patients with reversible or treatable causes may have a better prognosis compared to those with advanced or incurable conditions.
Response to Intervention:
The prognosis of cardiac tamponade is significantly influenced by the response to pericardiocentesis or surgical intervention.
Prompt drainage of pericardial fluid can rapidly improve hemodynamics and prevent complications, leading to better outcomes.
Pericarditis vs Cardiac Tamponade: Summary
In conclusion, while pericarditis and cardiac tamponade are both serious conditions affecting the pericardium, their prognoses differ based on their underlying pathophysiology, clinical course, and response to treatment. Pericarditis generally has a favorable prognosis with appropriate management, whereas cardiac tamponade represents a medical emergency requiring immediate intervention to prevent hemodynamic collapse and death. Timely recognition, accurate diagnosis, and prompt treatment are essential for optimizing outcomes and preventing complications in patients with pericardial conditions.
atment, and prognosis:
AspectPericarditisCardiac TamponadeSymptoms– Chest pain (sharp, stabbing, pleuritic) – Fever – Dyspnea – Pericardial friction rub – ECG changes (ST elevation, PR depression)– Beck’s triad: Hypotension, distended neck veins, muffled heart sounds – Pulsus paradoxus – Dyspnea – TachycardiaDiagnosis– Clinical evaluation – ECG changes – Pericardial friction rub – Echocardiography – Blood tests (e.g., inflammatory markers)– Clinical evaluation – Echocardiography (confirmatory) – Beck’s triad – Pulsus paradoxus – Chest X-ray – CT/MRI scansTreatment– NSAIDs (first-line) – Colchicine – Corticosteroids (severe cases) – Treat underlying cause – Rest and symptom management– Pericardiocentesis (emergency) – Volume expansion (fluids) – Surgical interventions (pericardial window, pericardiectomy)Prognosis– Generally favorable – Recurrences possible – Complications rare but possible– Requires prompt intervention – Prognosis depends on timeliness of treatment, underlying cause, and response to therapy© 2024 Moosmosis Organization
Check out this popular article on the heart blood flow pathway steps!
Have a Great Day!
Check out these popular articles
Circulatory System: Blood Flow Pathway Through the Heart
Ectoderm vs Endoderm vs Mesoderm
Circulatory System: Heart Structures and Functions
Ductus Arteriosus Vs Ductus Venosus Vs Foramen Ovale: Fetal Heart Circulation
Autocrine vs Paracrine vs Endocrine: What are the Differences?
Upper Vs Lower Respiratory System: Upper vs Lower Respiratory Tract Infections
Seven General Functions of the Respiratory System
Kidney Embryology & Development: Easy Lesson
Psychology 101: Crowd Psychology and The Theory of Gustave Le Bon
Cell Membrane Dynamics: Flippase Vs Floppase Vs Scramblase
Shoulder Abduction Muscles: Medical Anatomy and USMLE
Top Websites Like Sparknotes: 15 Free Sites and Resources Similar to Sparknotes
Cell Membrane Fluidity: Factors That Influence and Increase the Cell Membrane Fluidity
NBME 4, NBME 5, NBME 6 Internal Medicine Forms Answers and Explanations
Copyright © 2024 Moosmosis Organization: All Rights Reserved
All rights reserved. This essay first published on moosmosis.org or any portion thereof may not be reproduced or used in any manner whatsoever
without the express written permission of the publisher at moosmosis.org.
Please Like and Subscribe to our Email List at moosmosis.org, Facebook, Twitter, Youtube to support our open-access youth education initiatives!
Hey there, my friends! In this lesson, we explore pericarditis and cardiac tamponade which are two distinct cardiac conditions that can affect the pericardium, the sac-like structure surrounding the heart. While both conditions involve inflammation or fluid accumulation around the heart, they differ in their etiology, symptoms, diagnosis, treatment, and prognosis. anatomy, Biology, cell biology, education, health, medicine, stem, technology, aortic regurgitation, aortic stenosis, astrocyte, autonomic nervous system, biosignaling, blood flow, blood flow steps, brain, brain stem, capacitance, cardiac CT, cardiac MRI, cardiac tamponade, cardiologist, cardiology, cardiothoracic surgery, cardiovascular, central nervous system, cerebellum, cerebrum, chest pain, college, CT, demyelination, diagnosis, diastole, diastolic heart failure, doctor, ECG, ECHO, eeg, endocardium, enzyme, ependymal cells, first degree heart block, fMRI, G protein, GABA, GBS, glycine, graded potential, gray matter, guillain-barre syndrome, heart, heart block, heart failure, insurance, life, ligand, mcat, membrane receptor, microglia, mobitz, MRI, multiple sclerosis, myocardium, nerves, neuroimaging, neurology, neuron, neuroplasticity, neuroradiology, pericarditis, pericardium, periocardiocentesis, PET, physiology, prognosis, pulmonary flow, reflex, Scan, school, science, student, surgery, symptoms, synapse, systemic, systole, systolic heart failure, TAVR, third degree heart block, transduction, treatment, university, upper motor neuron, white matter Moosmosis