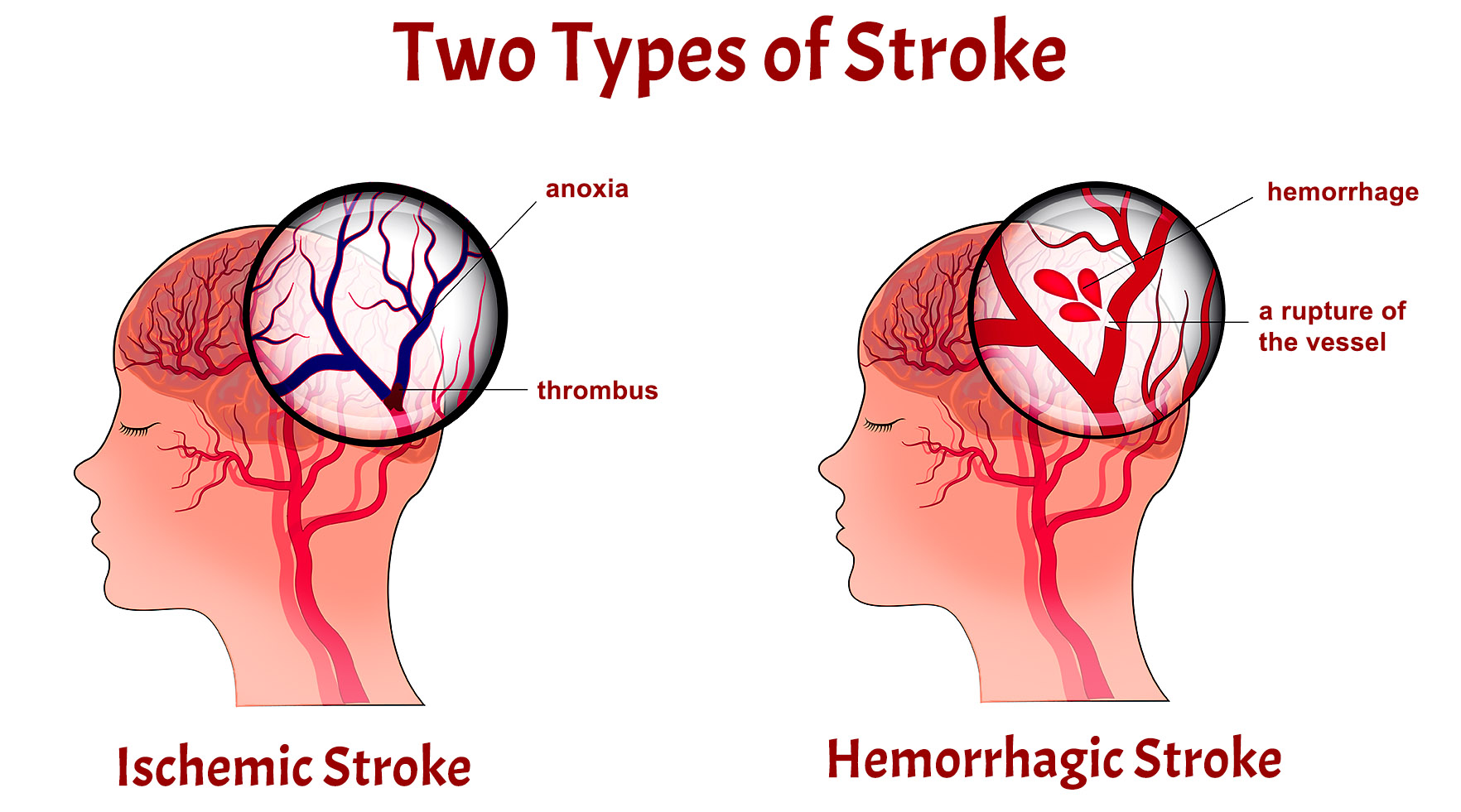
Strokes are a leading cause of disability and mortality worldwide, affecting millions of people each year. Two primary types of strokes, ischemic and hemorrhagic, differ in their underlying causes, symptoms, and treatments. Understanding the distinctions between these types is crucial for effective management and prevention in patients.
Symptoms: Ischemic Stroke vs Hemorrhagic Stroke
Ischemic Stroke Symptoms:
Ischemic strokes, constituting the majority of stroke cases, result from the obstruction of blood vessels supplying the brain. A hallmark of ischemic strokes is the sudden onset of weakness or numbness, typically affecting one side of the body. Speech and language difficulties, ranging from slurred speech to an inability to comprehend language, are common. Visual impairments, such as sudden blurriness or partial loss of vision, may also manifest. Additionally, severe headaches may occur, particularly when the stroke is attributed to vessel rupture. These symptoms collectively reflect the localized effects of diminished blood flow and oxygen delivery to specific brain regions.
Hemorrhagic Stroke Symptoms:
In contrast, hemorrhagic strokes originate from bleeding within the brain, creating a distinct clinical profile. A pronounced and intense headache is a characteristic symptom, often described as the most severe headache a patient has ever experienced. Nausea and vomiting can ensue, a consequence of increased intracranial pressure resulting from bleeding. Rapid loss of consciousness is more prevalent in hemorrhagic strokes, underscoring the acute impact of bleeding on overall brain function. Neurological deficits, including weakness or paralysis, are shared symptoms with ischemic strokes, though the underlying cause in hemorrhagic strokes is hemorrhage rather than ischemia.
Comparison:
The onset and progression of ischemic and hemorrhagic strokes represent a crucial point of distinction. Ischemic strokes typically exhibit a more gradual onset, affording a wider time window for medical intervention. In contrast, hemorrhagic strokes have a sudden and rapid onset, necessitating urgent medical attention. Severe headache is a commonality in both stroke types, yet its prominence is heightened in hemorrhagic strokes. Neurological deficits, including motor impairments, are evident in both, emphasizing the impact on physical function. Notably, ischemic strokes more frequently result in speech and language impairments, whereas hemorrhagic strokes can also affect communication abilities.
Diagnosis: Ischemic Stroke vs Hemorrhagic Stroke
Diagnostic Methods for Ischemic Stroke:
Ischemic strokes, characterized by a disruption of blood flow to the brain, necessitate rapid and precise diagnostic measures. Neuroimaging techniques, such as computed tomography (CT) scans and magnetic resonance imaging (MRI), are paramount in identifying ischemic strokes. CT scans, often the initial diagnostic tool, can reveal early signs of ischemia, while MRI provides a more detailed view, aiding in the determination of the location and extent of the ischemic event. Furthermore, the utilization of vascular imaging techniques, such as CT angiography or magnetic resonance angiography, allows clinicians to identify potential sources of emboli or thrombosis contributing to the ischemic event.
Diagnostic Approaches for Hemorrhagic Stroke:
Contrary to ischemic strokes, hemorrhagic strokes result from bleeding within the brain. The urgency in diagnosing hemorrhagic strokes is paramount due to the potential for rapid deterioration. Non-contrast CT scans are typically the first-line diagnostic tool for detecting hemorrhagic strokes, providing immediate visualization of bleeding within the brain. Cerebral angiography may be employed to identify the precise location and cause of bleeding. Lumbar puncture, although less common, can also aid in differentiating hemorrhagic strokes from other neurological conditions when imaging alone does not provide conclusive results.
Comparison:
Both ischemic and hemorrhagic strokes may present with similar initial symptoms, underscoring the importance of swift and accurate diagnosis. However, the key distinction lies in the imaging findings. While CT scans are vital for identifying bleeding and ischemic changes in both types of strokes, the use of advanced imaging modalities, such as MRI and vascular imaging, is more pronounced in ischemic stroke diagnosis. The urgency in diagnosing hemorrhagic strokes necessitates a prompt and precise interpretation of non-contrast CT scans to guide immediate intervention.
CT heads showing ischemic stroke and hemorrhagic stroke
Treatment: Ischemic Stroke vs Hemorrhagic Stroke
Treatment Approaches for Ischemic Stroke:
Ischemic strokes, arising from the occlusion of blood vessels supplying the brain, demand swift and targeted interventions to restore blood flow and mitigate neurological damage. Thrombolytic medications, such as tissue plasminogen activator (tPA), are often administered intravenously to dissolve blood clots causing the ischemia. Antiplatelet medications, including aspirin, prevent further clot formation and reduce the risk of recurrent ischemic events. In cases where large vessel occlusion is identified, mechanical thrombectomy, involving the removal of clots using catheter-based procedures, has emerged as a revolutionary intervention.
Treatment Strategies for Hemorrhagic Stroke:
Hemorrhagic strokes, characterized by bleeding within the brain, necessitate a different therapeutic approach due to the increased risk of further bleeding and neurological deterioration. Surgical interventions may be required to address the underlying cause of bleeding, such as aneurysm clipping or coiling in the case of an aneurysmal hemorrhage. Medications to control blood pressure are crucial to prevent re-bleeding, and supportive care aims to manage associated symptoms and complications. In certain instances, transfusions or medications to reverse anticoagulant effects may be administered.
Comparison:
While both types of strokes share the goal of preventing secondary complications and optimizing recovery, the treatments diverge significantly due to the contrasting nature of ischemic and hemorrhagic events. The administration of thrombolytic agents and antiplatelet medications is a cornerstone in ischemic stroke management, focusing on reestablishing blood flow and preventing further clot formation. In contrast, hemorrhagic strokes require a cautious approach to avoid exacerbating bleeding. The utilization of surgical interventions and blood pressure control becomes paramount to mitigate the risk of re-bleeding.
Prognosis: Ischemic Stroke vs Hemorrhagic Stroke
Prognostic Factors in Ischemic Stroke:
Ischemic strokes, resulting from a disruption of blood flow to the brain, present a spectrum of prognostic factors. Timeliness in initiating treatment is critical, and patients who receive thrombolytic therapy within the recommended window often experience better outcomes. The location and size of the infarcted area, as well as the extent of neurological deficits, play significant roles in determining prognosis. Rehabilitation interventions and post-stroke care, including physical and occupational therapy, contribute to recovery and influence long-term outcomes. Additionally, comorbidities such as hypertension and diabetes can complicate the prognosis of ischemic strokes, underscoring the importance of comprehensive post-stroke management.
Prognostic Considerations in Hemorrhagic Stroke:
Hemorrhagic strokes, marked by bleeding within the brain, introduce unique challenges in prognosis. The severity and location of the hemorrhage influence outcomes, with deep-seated bleeds often associated with poorer prognosis. The rapidity of medical intervention is crucial, and patients who receive prompt care may exhibit more favorable outcomes. However, the risk of re-bleeding and complications related to increased intracranial pressure can impact long-term recovery. Rehabilitation and supportive care, tailored to the specific needs of individuals with hemorrhagic strokes, play a pivotal role in determining prognosis.
Comparison:
Comparing the prognosis of ischemic and hemorrhagic strokes reveals both similarities and distinctions. In general, ischemic strokes, particularly those with smaller infarcts and less severe neurological deficits, tend to have more favorable prognoses. The ability to receive thrombolytic therapy and engage in comprehensive rehabilitation contributes significantly to recovery. Hemorrhagic strokes, on the other hand, often entail a higher risk of morbidity and mortality, influenced by factors such as the location of bleeding and the challenges associated with preventing re-bleeding.
Challenges and Emerging Trends:
Challenges in predicting prognosis include the variability in individual responses to treatment, the influence of pre-existing conditions, and the complexity of neurological recovery. Emerging trends in stroke research explore predictive modeling using advanced imaging techniques and biomarkers to refine prognostic assessments. Additionally, innovations in telemedicine and virtual rehabilitation programs show promise in optimizing post-stroke care and enhancing recovery trajectories.
Conclusion:
In conclusion, the prognosis of ischemic and hemorrhagic strokes is shaped by a multitude of factors, including the size and location of the cerebrovascular event, the timeliness of medical interventions, and the effectiveness of rehabilitation. While ischemic strokes generally exhibit more favorable outcomes, the prognosis varies widely, emphasizing the need for individualized care. As research continues to uncover novel prognostic indicators and therapeutic strategies, the landscape of stroke management is poised for further advancements, ultimately improving the quality of life for those affected by these critical neurological events.
Summary table: Ischemic Stroke vs Hemorrhagic Stroke
AspectIschemic StrokeHemorrhagic StrokeSymptoms– Sudden weakness or numbness on one side– Sudden and severe headache– Speech and language difficulties– Nausea and vomiting– Vision impairment– Loss of consciousness– Severe headache– Neurological deficits (weakness/paralysis)Diagnosis– CT scans and MRI for identifying location– Non-contrast CT scans for immediate visualization– Vascular imaging for clot detection– Cerebral angiography for precise bleeding location– Time-sensitive interventions for thrombolysis– Lumbar puncture for specific cases– Identification of potential emboli or thrombosisTreatment– Thrombolytic medications (tPA) for clot dissolution– Surgical interventions (clipping, coiling)– Antiplatelet drugs (aspirin) for clot prevention– Blood pressure control to prevent re-bleeding– Mechanical thrombectomy for clot removal– Supportive care for symptom management– Rehabilitation for recovery and lifestyle changes– Transfusions or medications to reverse anticoagulationPrognosis– Favorable outcomes with timely intervention– Higher risk of morbidity and mortality– Rehabilitation aids recovery and lifestyle changes– Prognosis influenced by location and severity of bleed– Comorbidities may complicate prognosis– Risk of re-bleeding and complications impact recovery© 2024 Moosmosis Organization
Check out these popular articles
Circulatory System: Blood Flow Pathway Through the Heart
Ectoderm vs Endoderm vs Mesoderm
Circulatory System: Heart Structures and Functions
Ductus Arteriosus Vs Ductus Venosus Vs Foramen Ovale: Fetal Heart Circulation
Autocrine vs Paracrine vs Endocrine: What are the Differences?
Upper Vs Lower Respiratory System: Upper vs Lower Respiratory Tract Infections
Seven General Functions of the Respiratory System
Kidney Embryology & Development: Easy Lesson
Psychology 101: Crowd Psychology and The Theory of Gustave Le Bon
Cell Membrane Dynamics: Flippase Vs Floppase Vs Scramblase
Shoulder Abduction Muscles: Medical Anatomy and USMLE
Top Websites Like Sparknotes: 15 Free Sites and Resources Similar to Sparknotes
Cell Membrane Fluidity: Factors That Influence and Increase the Cell Membrane Fluidity
Copyright © 2024 Moosmosis Organization: All Rights Reserved
All rights reserved. This essay first published on moosmosis.org or any portion thereof may not be reproduced or used in any manner whatsoever
without the express written permission of the publisher at moosmosis.org.
Please Like and Subscribe to our Email List at moosmosis.org, Facebook, Twitter, Youtube to support our open-access youth education initiatives!
Strokes are a leading cause of disability and mortality worldwide, affecting millions of people each year. Two primary types of strokes, ischemic and hemorrhagic, differ in their underlying causes, symptoms, and treatments. Understanding the distinctions between these types is crucial for effective management and prevention in patients. anatomy, Biology, cell biology, education, health, medicine, stem, technology, autonomic nervous system, bleeding, brain, brain bleed, brain stem, brain surgery, central nervous system, cerebellum, cerebrum, college, ct head, epidural hematoma, gray matter, hemorrhage, hemorrhagic stroke, interventional radiology, ischemic stroke, life, mcat, MRI, MRI brain, nerves, neurology, neuron, neuroradiology, neuroscience, neurosurgery, parasympathetic, peripheral nervous system, physiology, radiology, reflex, school, science, somatosensory, stretch reflex, stroke, student, subarachnoid hemorrhage, subcortical cerebrum, subdural hematoma, surgery, sympathetic, TIA, transient ischemic attack, university, upper motor neuron, white matter Moosmosis